Face coverings are an essential tool in decreasing the spread of COVID-19, but for those who are hearing impaired, they can pose significant challenges to communication. Maura K. Cosetti, MD, Director of the Ear Institute of the New York Eye and Ear Infirmary of Mount Sinai, specializes in diagnosis and treatment of hearing loss and attests to the significant impact that face coverings have on communication in the COVID era.
“The challenges are multifactorial—from medical to environmental as well as social and
behavioral,” says Dr. Cosetti. “Our world has changed dramatically and our communications style must change accordingly, especially when interacting with patients who are hearing impaired.”
Even individuals with perfect hearing rely on facial expressions and lip movements to understand speech. When a face covering obscures half of the face, it greatly impacts our
ability to visualize these cues and communicate. Face coverings also affect the attenuation of sound, making it difficult for someone who is hard of hearing to differentiate between words—particularly those with “t” or “ch” sounds.
Communicating outdoors (such as at sidewalk restaurants) is also more difficult due to the addition of environmental background noise. These outdoor sounds make it more difficult for individuals with hearing loss to understand and participate in conversations. In the hospital, increased use of machines to create negative pressure—and reduce transmission of viral particles—creates loud background noise, making speech harder to understand. Recent data, published in the November/December 2020 issue of Ear and Hearing, demonstrated that individuals with hearing loss have increased anxiety regarding verbal communication during the COVID-19 pandemic, citing face masks and decreased access to audiology services as major concerns.
Hearing-impaired individuals also have other unique struggles with wearing face coverings. “Ear ‘real estate’ is an issue,” explains Dr. Cosetti. “Imagine having a hearing aid, glasses, and the loops from a face mask all in the same location. Many of my patients have had expensive hearing aids fall on the floor, and others have lost them entirely. Some are even hesitant to wear their hearing aids because of these issues.
Is COVID-19 Exacerbating Hearing Loss?
Researchers are still trying to understand the effects of COVID-19 on hearing loss, balance, and tinnitus. Initial research, published October 23, 2020, in European Archives of Oto-Rhino-Laryngology, suggests these symptoms may be common in patients with COVID-19 infection. In addition, some medications like hydroxychloroquine and ribavirin that have been used to
treat the virus can be toxic to our hearing. Furthermore, uncharted levels of stress during the
pandemic may attribute to the rise in tinnitus, which has long been linked to anxiety and depression.
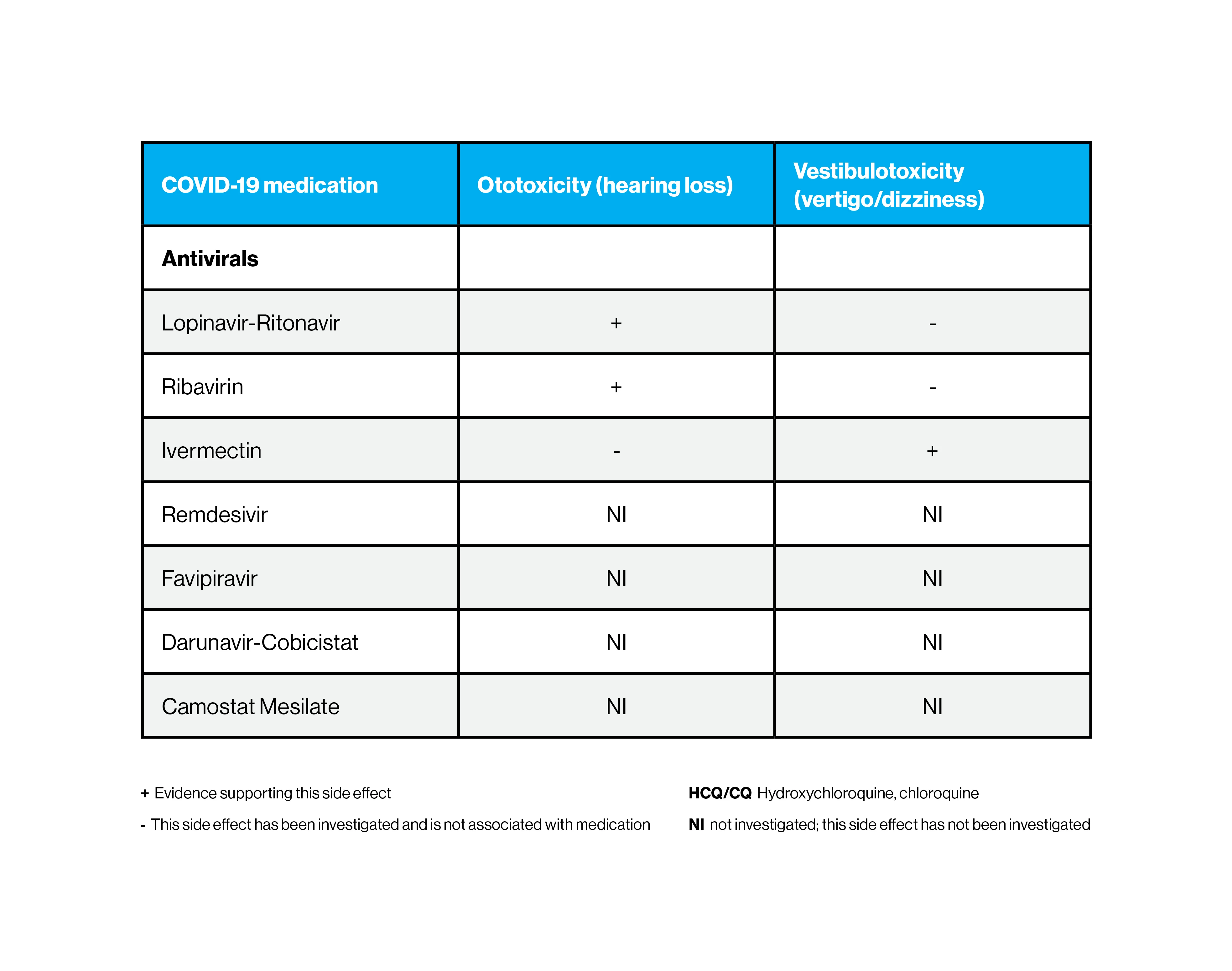
Antiviral medications that are used to treat COVID-19 and their impact on hearing loss
“We have known for some time that sensory hearing loss can result from other types of viral infections, and it appears that COVID-19 may be similar. With all of these potential causes
acting together, this rise in tinnitus, hearing loss, and dizziness does not seem surprising,” says Dr. Cosetti. “I expect we will learn a great deal more about the hearing and balance effects of COVID infection in the coming months and years.”
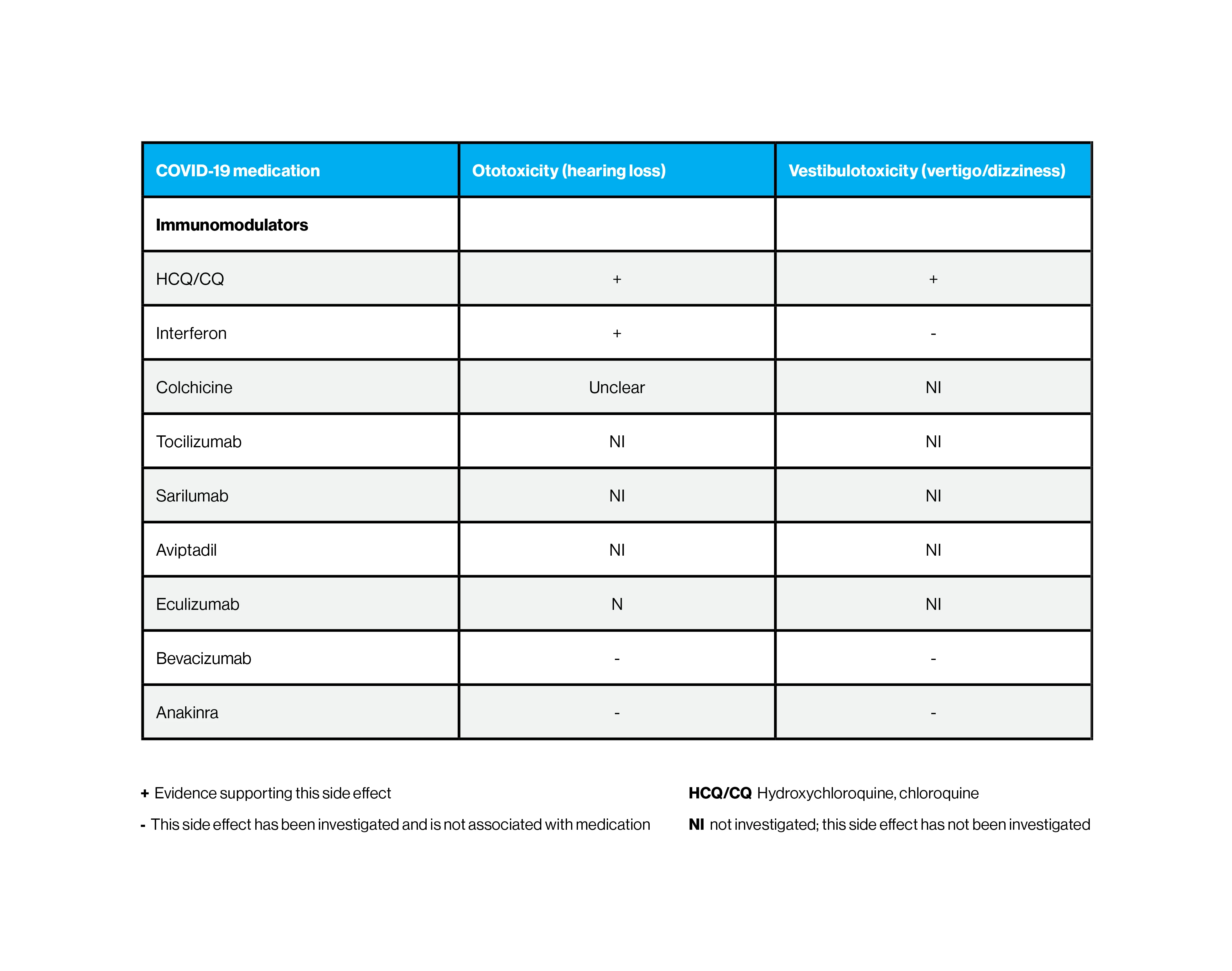
Immunomodulators that are used to treat COVID-19 and their impact on hearing loss
The good news, however, is that the pandemic may be shining a light on the often “invisible” disability of hearing loss. For those who are hard of hearing—and their family members—the challenges related to communication may seem more obvious. Typically more than 80 percent of individuals with hearing loss decide not to be treated. However, the pandemic has inspired many who are struggling to find a better way to communicate. “We have an opportunity to address the tremendous gap in individuals who could benefit from hearing aids and devices like cochlear implants,” says Dr. Cosetti.
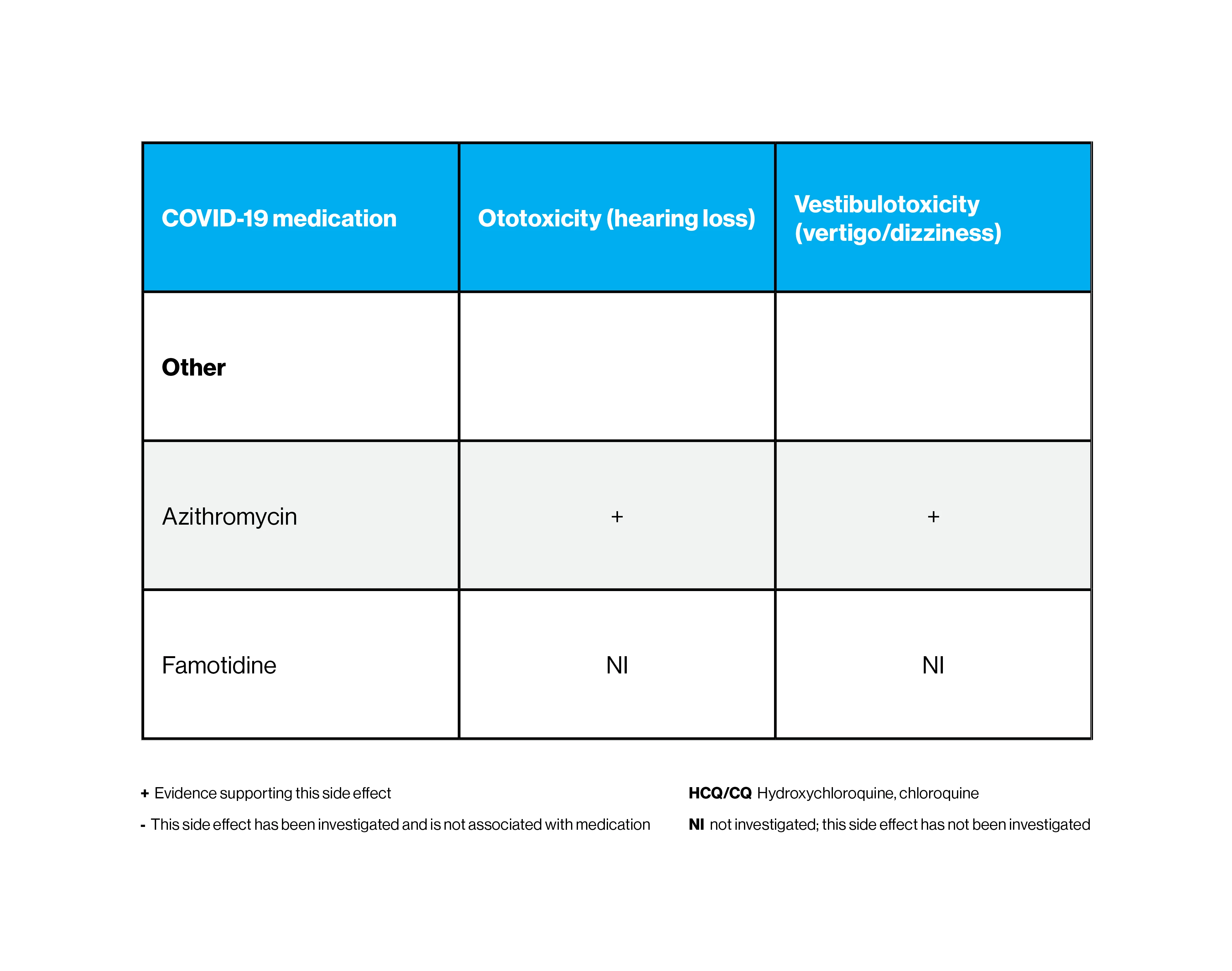
Other medications that are used to treat COVID-19 and their impact on hearing loss
How Providers Can Help Their Hearing-Impaired Patients
During the COVID-19 era, providers should be sensitive to the challenges of communicating with individuals who have hearing impairments. Whether you are seeing a patient in the office or through telemedicine, here are some tips to ensure an engaging—and effective— visit.
Dr. Cosetti discusses what she learned as an otologist working in a COVID-19 intensive care unit.
- 1.
Wear a clear mask. It can be difficult to understand providers when they wear N95 or surgical masks. Otologists at Mount Sinai use masks that have a clear transparent material over the mouth so patients can read their lips safely.
- 2.
Lower your voice. It may seem counterintuitive but talking loudly actually distorts speech more. Focus on speaking clearly and phrase questions to include more information. For example, instead of asking “how is your breathing?” say “are you having trouble taking deep breaths?”
- 3.
Reduce background noise. To reduce the spread of COVID-19, many businesses and medical practices are using loud air filtration systems. Find a location that limits external sounds. If you are communicating virtually, find a quiet place at home and shut the door. There are also several apps that can help eliminate unwanted noise.
- 4.
Use technology. Speech-to-text apps like Live Transcribe, Otter.ai., and Web Captioner use automatic speech recognition to transcribe your conversation. It is very helpful for hearing-impaired patients to have a visual transcript of your meeting.
- 5.
Get confirmation. Engage in effective communication by confirming if the patient understands you. For virtual visits or telemedicine, try using the chat function.
- 6.
Look at your patient. Studies show that medical providers may focus their attention on the chart or computer screen. Make eye contact throughout the session—hearing-impaired individuals need to see your face.
Featured
Maura K. Cosetti, MD
Assistant Professor of Otolaryngology—Head and Neck Surgery
