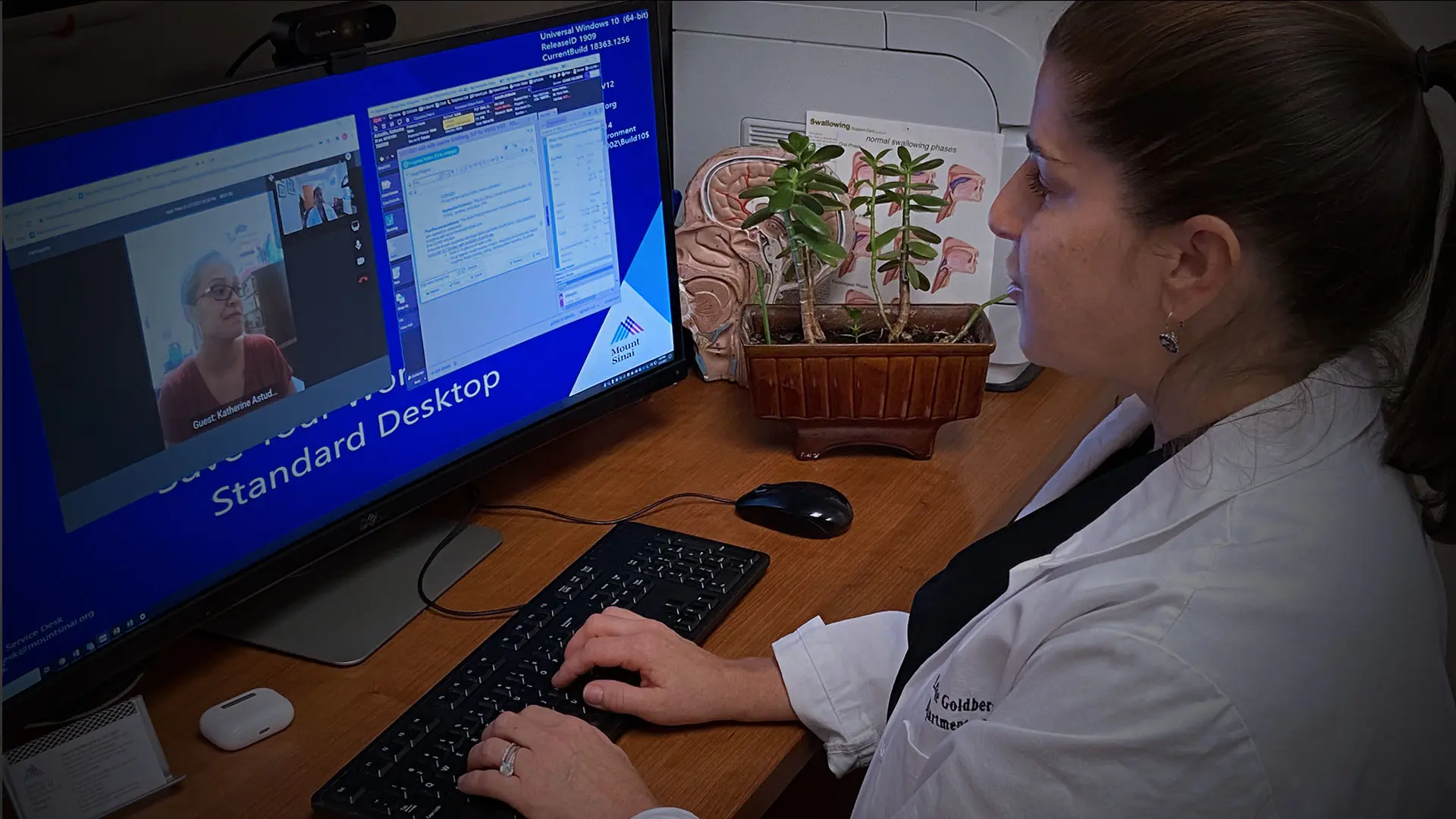
When New York City became the epicenter of the COVID-19 pandemic, Leanne Goldberg, MS, CCC-SLP, switched from in-person speech language pathology evaluations at the Grabscheid Voice and Swallowing Center of Mount Sinai to virtual appointments to reduce her patients’ risk of infection. Although the move posed a few challenges—instrumental assessments of larynx and swallow function, laryngeal massage, and device demonstrations became difficult or impossible to do—she believes it worked out relatively well given the circumstances.
“We saw there were benefits to telemedicine, such as schedule flexibility, being able to serve patients who were not able to come to Mount Sinai due to the pandemic, and, importantly, patients were able to have their appointments in an environment that was more comfortable for them,” explains Ms. Goldberg, who is Director of Speech Language Pathology at the Grabscheid Voice and Swallowing Center of Mount Sinai. “It occurred to us there might be certain demographics or diagnoses where we could maintain this modality as an option.”
Curious as to the viability of offering virtual consultations in a post-pandemic context, Ms. Goldberg has launched the Telemedicine Outcome Survey to gauge patient satisfaction and impacts. The survey is open to any patient who participated in three telemedicine sessions with a Mount Sinai Speech-Language Pathologist. Once enrolled, participants complete the Short Assessment of Patient Satisfaction questionnaire either by using a link sent to their phones or, if preferred, through a phone interview with a Mount Sinai medical student. The survey measures their degree of satisfaction or dissatisfaction with seven consultation-related metrics, including duration of consultations, information they received, and their outcomes.
Patients with varied pathologies were seen via telemedicine, including treatment for voice disorders, chronic cough, swallowing disorders and transgender voice modification. Although the survey is ongoing, Ms. Goldberg says preliminary results from 70 respondents (median age 50.5), have provided invaluable insights as to the efficacy of telemedicine consultations. Three metrics earned high scores—overall satisfaction (a score of 22.46 out of 28), satisfaction with efficacy of care (3.72 out of four), and thoroughness of provider—while two—length of visit (2.22) and explanations (2.52)—earned the lowest scores.
“Based on these preliminary results, the level of satisfaction is approximately the same as what we see with in-person consultations, which is very positive,” Ms. Goldberg says. “This, combined with the fact that reimbursement from insurance companies is comparable to that for in-person consultations, suggests that telemedicine is a viable treatment option for our patients and can be particularly important for those who live far away, or who are not ambulatory.”
Ms. Goldberg plans to explore other aspects of telemedicine among patients as participant recruitment continues, specifically whether age, gender, and diagnosis impact satisfaction and efficacy. The team has also noted benefits of a hybrid treatment model, which would include both telemedicine and in-person visits. “There will always be patients we will need to see in office, such as those who may benefit from laryngeal massage, and those who prefer in person treatment, but the more data we gather, the more insights we can gain as to which conditions and patients might be well served by telemedicine,” Ms. Goldberg says.
Featured

Leanne Goldberg, MS, CCC-SLP
Director of Speech Language Pathology Grabscheid Voice and Swallowing Center of Mount Sinai