Post-COVID-19 complications are on the rise. Ever since the initial flattening of the curve of infections in May 2020, otolaryngologists throughout the Mount Sinai Health System have seen an increasing number of patients with a history of COVID-19 infection present with voice and breathing complications. At least once a week physicians evaluate patients with difficulty breathing who had previously been intubated due to COVID-19, as well as others who, despite experiencing only mild symptoms from the virus, report chronic cough, hoarseness, and difficulty swallowing.
To better address the needs of this growing patient population, physicians within the Department of Otolaryngology - Head and Neck Surgery at the Icahn School of Medicine at Mount Sinai have formed a COVID-19 Airway Collaborative to research the effects of the virus on the upper airway structures such as the larynx and trachea.
“We have seen viruses impact the upper airway before, but never as significantly as COVID-19,” says Diana Kirke, MD, Assistant Professor in the Department of Otolaryngology - Head and Neck Surgery at the Icahn School of Medicine. “Even in the worst flu season, our specialty would not be seeing this many patients each week.”

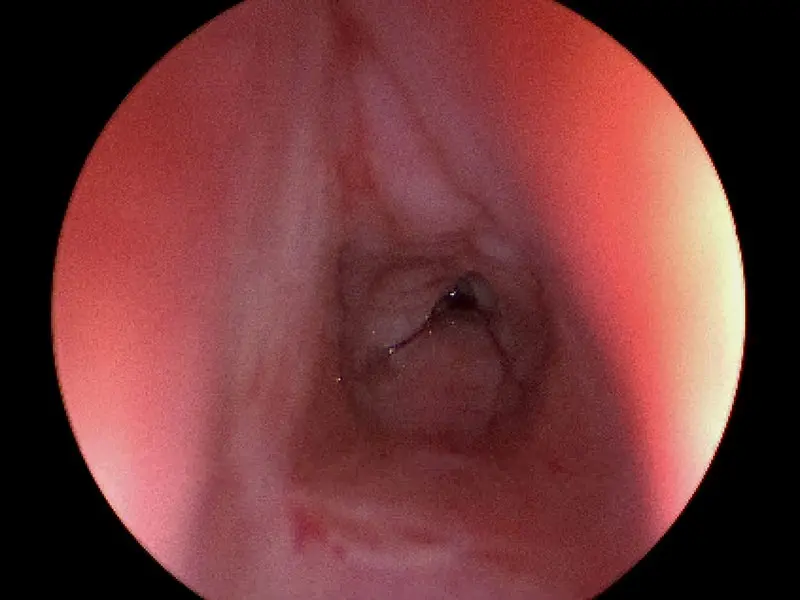
A patient that was previously intubated for COVID-19 who has developed posterior glottic stenosis.
A patient that was previously intubated for COVID-19 who has developed subglottic stenosis.
Promoting Immediate Intervention by Educating Physicians
A critical objective of Mount Sinai researchers is to educate other physicians to refer patients to an otolaryngologist if they have recovered from COVID-19 and continue to have upper airway complications for more than a week.
Notably, the complications are occurring across the spectrum of disease, often puzzling physicians. For example, in May, otolaryngologists at Mount Sinai first began seeing individuals who had been intubated in March for a long period of time or had a tracheotomy present with conditions that affected the trachea, epiglottis, and larynx, such as posterior glottic stenosis, tracheal stenosis, vocal fold paralysis, and vocal cord immobility. Soon after, patients who had not been intubated—and had mild to moderate disease that did not warrant hospitalization—began to present with chronic cough, vocal changes, or difficulty swallowing. These mild-to-moderate cases present a hurdle in identifying patients with post-COVID-19 laryngeal complications as some individuals may not know they had the virus.
“If anyone has a change in the way they breathe, talk, or swallow, their upper airway should be assessed,” says Dr. Kirke.
Individuals who have mild or moderate complications can greatly improve their quality of life with modalities like speech and language therapy, while those with more severe issues often require surgical procedures like balloon dilation or even a tracheal resection.
For patients with significant shortness of breath, even if it is only on exertion, it is critical not to ignore the symptoms as many end up needing emergency procedures.
“People often say, I did not realize how important my voice was until I lost it,” says Dr. Kirke, “but communication is central to everything we do.”

Dr. Kirke consults with a patient following stroboscopic and swallowing assessment.
Using a Multidisciplinary Approach to Address Laryngeal Complications
As part of a large Health System, Mount Sinai otolaryngologists have the resources to collaborate closely with multiple specialty services like pulmonology and thoracic surgery to address patient concerns. Dr. Kirke and her colleagues are also working closely with the Center for Post-COVID Care at Mount Sinai-Union Square to provide laryngology services.
Ongoing research is also providing clues. Until now, the lower respiratory tract was thought to be the primary target for COVID-19—studies have shown the virus enters the cells by attaching to angiotensin-converting enzyme 2 (ACE2)—but the upper airway and lower respiratory tract are inextricably linked. The cells being attacked are also present in the upper respiratory tract.
“This concept of a unified airway is not well known outside of the pulmonary and ear, nose, and throat specialties. However, we believe this idea is of interest to the wider medical community because some of the laryngeal complications that are presenting may be mistaken for ongoing lower respiratory tract disease,” explains Dr. Kirke.
Dr. Kirke believes that cells in the lower respiratory tract are similar to those in the upper airway and that is why we are seeing an increase in laryngeal complications. Mount Sinai researchers are exploring this hypothesis. While post-mortem studies of COVID-19 patients have focused primarily on the lower respiratory tract, physicians are beginning to study tissue samples in the upper airway taken from tracheal resections. Additional studies are also looking at intubation tube size and its effect on post-COVID-19 complications.
Mount Sinai is uniquely poised to study these laryngeal complications due to the sheer volume of COVID-19 patients treated throughout the eight hospitals of the Health System. Being in the eye of the storm has provided invaluable lessons about what symptoms to look for post-COVID-19 infection and which research to focus on to improve airway management for any future waves of COVID-19 or other viruses that may occur.
Featured

Diana Kirke, MD
Assistant Professor of Otolaryngology—Head and Neck Surgery
