A case review by a team at the Icahn School of Medicine at Mount Sinai highlighted the crucial role of endocrinologists in the assessment and management of patients with adrenocortical carcinoma (ACC), a rare and aggressive form of cancer. The review was presented in 2024 by Alice C. Levine, MD, Professor of Medicine (Endocrinology, Diabetes and Bone Disease) and Rachel Sheskier, MD, Assistant Professor of Medicine (Endocrinology, Diabetes, and Bone Disease). Mount Sinai has a long history and exceptional expertise in treating adrenal disease and receives referrals from across the United States for ACC, which affects only one to two people per million in the population.
“Since the establishment of the Adrenal Center at Mount Sinai around 2010, a surprising number of our referrals have turned out to be adrenal cortical cancer. In fact, last year we treated seven cases,” Dr. Levine says. “So, while this is a very rare cancer, it is being caught more often as a side effect of many more people having abdominal imaging. As we have become more experienced, we not only got better at it, but we are learning the nuances of the disease and its treatment. That precipitated our research efforts and our efforts to clinically streamline a multidisciplinary approach.”
Dr. Levine presented the review of ACC cases, titled “The Role of the Endocrinologist in the Diagnosis and Management of Adrenocortical Carcinoma: A Case-Based Review”, to the Endocrine Society in Boston in June 2024. The aim of the review was to contrast two cases, one managed by oncology alone and another managed by both oncology and endocrinology. The review’s recommendations were based on evidence from randomized prospective clinical studies, cohort studies, cross-sectional and case-based studies, and expert opinion.
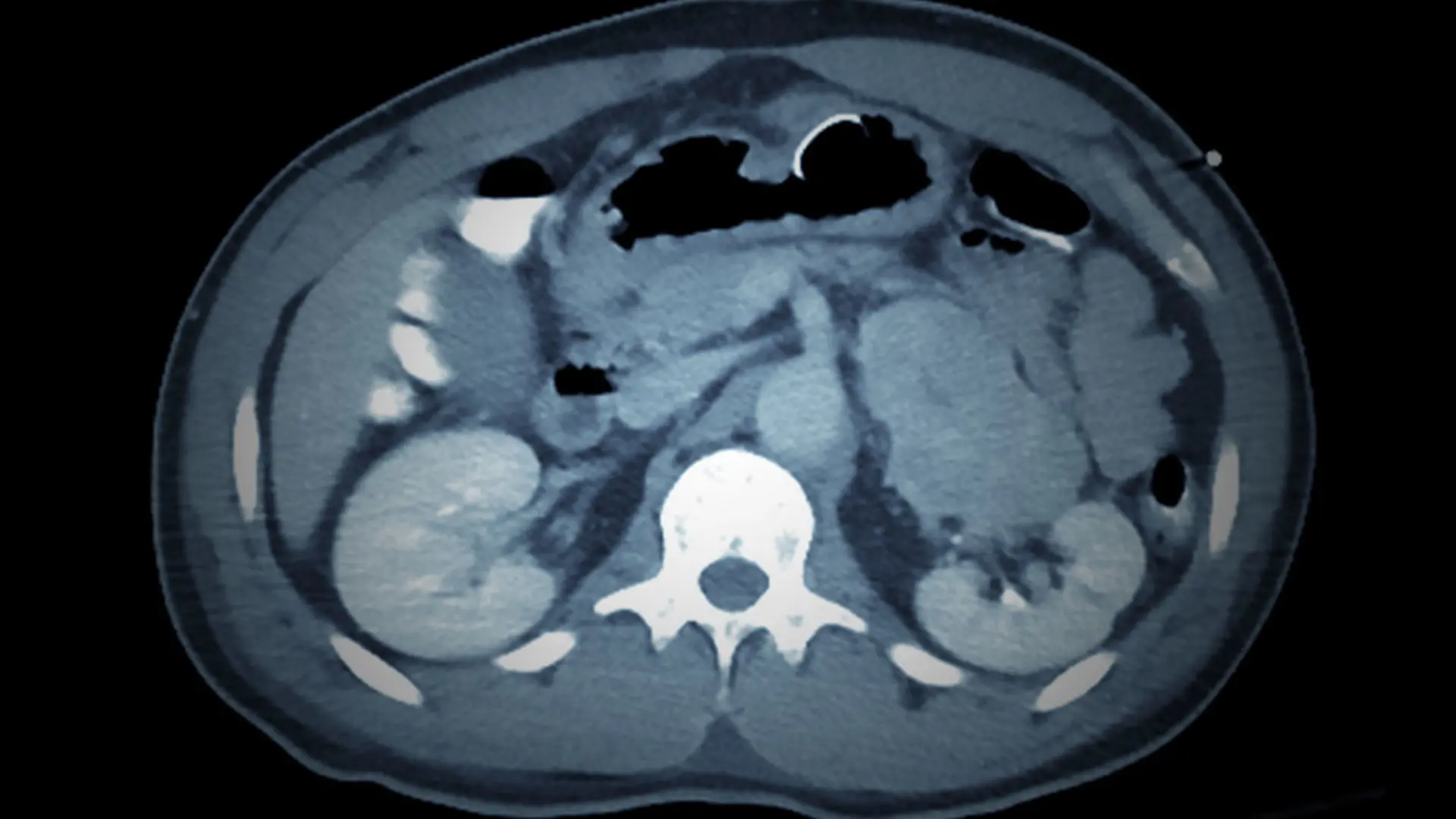
The first patient, a 40-year-old man with no significant medical history, presented to the Emergency Department for evaluation of abdominal pain. Imaging revealed a right adrenal 8 cm mass. The patient was then referred to oncology for evaluation due to suspicion for ACC. The oncologist obtained a baseline endocrine workup, including adrenocorticotropin hormone, cortisol, and prolactin. The patient was then referred to a urologic oncology surgeon for adrenalectomy.
A more comprehensive preoperative hormonal workup would have been preferable, the review said. More than half of ACC patients have clinical evidence of hormonal excess, most prominently hypercortisolism. Abnormal hormonal precursors and disorganized steroidogenesis are also hallmarks of ACC. Measurement of steroid precursors, more robust assessment for cortisol excess, and measurement of plasma metanephrines to rule out pheochromocytoma would have been helpful in this patient. Pheochromocytoma must be ruled out prior to subjecting a patient to anesthesia and surgery as those procedures can precipitate a pheo crisis, a potentially life-threatening condition. In addition, elevations in cortisol and especially in precursors would strongly point to a diagnosis of ACC preoperatively. Finally, if there is evidence of even mild hypercortisolism preoperatively, it alerts the multidisciplinary team that the patient will need postoperative glucocorticoid replacement therapy.
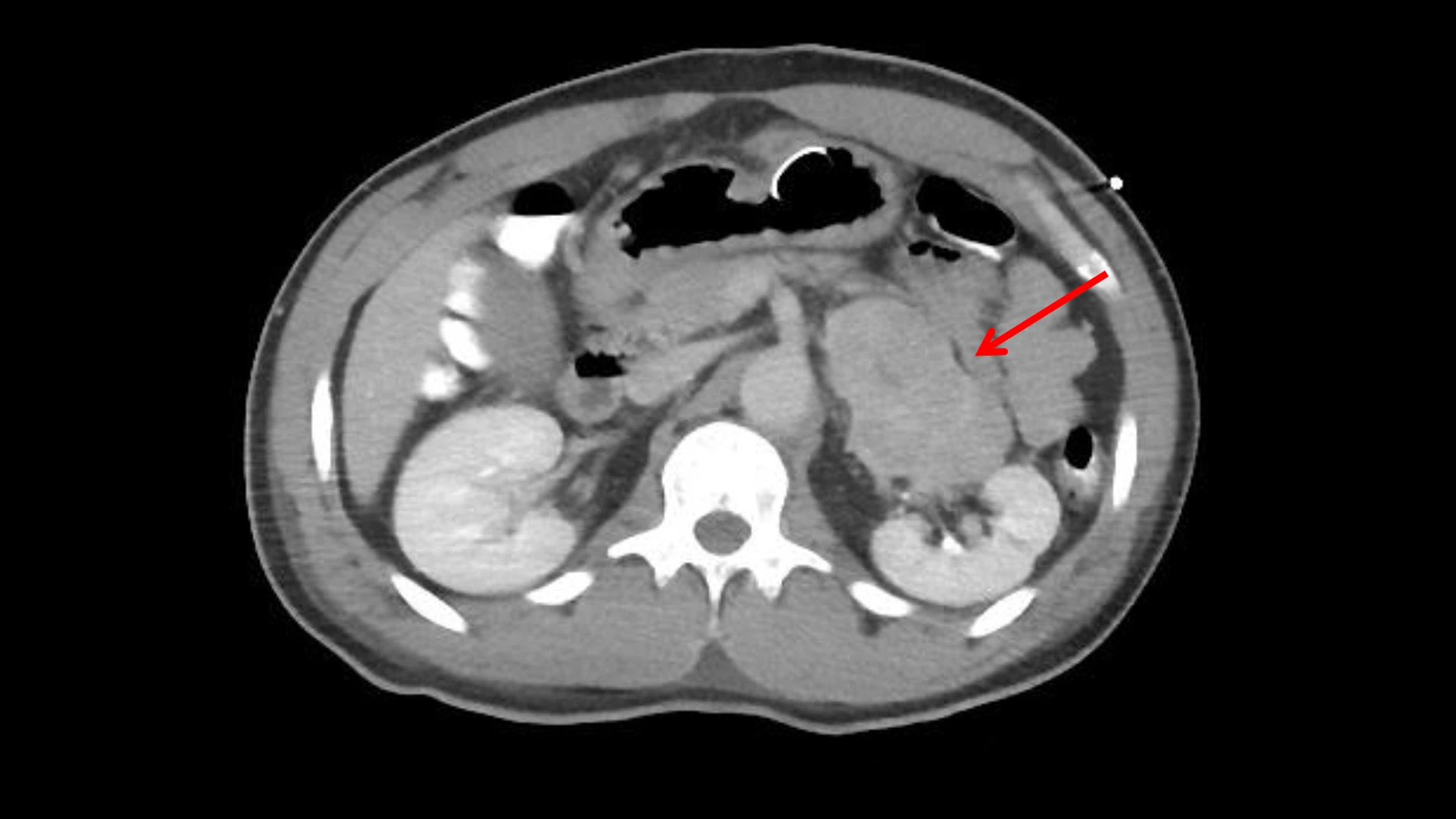
Adrenocortical carcinoma is adjacent to the left kidney on the CT image.
“While this is a very rare cancer, it is being caught more often as a side effect of many more people having abdominal imaging. ”
Alice C. Levine, MD
A better preoperative assessment to determine the risk of ACC would have also helped determine the type of surgery chosen. The patient underwent robotic-assisted laparoscopic right adrenalectomy, while a strong suspicion of ACC might have led the surgeon to perform en bloc resection via open surgery instead to avoid any possible spillage of cancer cells.
Three months after adrenalectomy, the patient went to the oncologist for follow-up. He was deemed to have ACC with high risk for recurrence, and adjuvant mitotane therapy was initiated. Mitotane, a drug with unique pharmacokinetics and an array of side effects, is the only medication approved by the Food and Drug Administration for the treatment of ACC. While this medication is often prescribed and managed by oncology, the nuances of glucocorticoid replacement and assessment for endocrinopathies associated with mitotane necessitate the continued involvement of the endocrinologist in the patient’s care team. Beyond monitoring for potential side effects, the continued surveillance of the hormonal profile, hormone precursors, and symptoms by the endocrinologist is paramount as these may change depending on the progression and/or recurrence of disease, and also with changes in mitotane blood levels, which in turn may require adjustments in treatment.
The second case describes a patient with ACC managed by oncology and endocrinology. A 47-year-old man with thyroid nodules and hypothyroidism presented following an incidental finding of an adrenal mass on imaging. The patient was referred for surgical resection and specialized endocrinology care at an adrenal center in a large tertiary hospital.
Postoperatively, the patient was medically managed with mitotane and hydrocortisone. However, five months after adrenalectomy, the patient showed evidence of recurrence of ACC in the adrenal surgical bed. The patient underwent resection of the recurrence, and his metastatic ACC was treated with radiation therapy and pembrolizumab, which was transitioned to nivolumab/ipilimumab that was discontinued after several months due to side effects. He was then treated with etoposide, doxorubicin, and cisplatin as determined by oncology, and adjuvant mitotane was continued.

Rachel Sheskier, MD, left, and Alice C. Levine, MD
While receiving these treatments, the patient experienced several mitotane side effects, which were managed by his endocrinologist. The side effects were symptomatic hypoaldosteronism (hypotension, high potassium, and high plasma renin activity) requiring fludrocortisone supplementation, hypogonadism treated with testosterone replacement, and increasing thyroid stimulating hormone (TSH) treated with levothyroxine. This case demonstrates the importance of continued hormonal assessment. Management of symptoms due to endocrinopathies allowed the patient to maintain mitotane dosing and levels in the therapeutic range to treat his ACC.
“The hormonal aspect plays a big role in adrenal cortical cancer in terms of making people sick and making them not be able to tolerate cancer treatments, including mitotane. Our job as endocrinologists is to optimize their endocrine status,” Dr. Sheskier says. “ACC is a difficult cancer to treat in that is has an additional factor, which is that it makes hormones. So if you have hormonal excess, that's adding to the morbidity and mortality of medical situation. That's the part where an endocrinologist can be useful. You don't want somebody to expire from an endocrinopathy, because that can be treated and managed.”
Dr. Levine, a leader in the study and treatment of adrenal disorders, is also co-Director of Mount Sinai’s Endocrinology Fellowship, the largest and most diverse in the nation in terms of clinical and research experience. For her overall achievements, Dr. Levine is the recipient of the 2025 Laureate Award for “Outstanding Educator” from the Endocrine Society, one of the top honors in the field. She is a highly sought-after speaker at national and international meetings for her research into prostate cancer and adrenal diseases. Her publications are frequently cited, and she has edited three textbooks that serve to educate endocrinologists in the fields of hormonal neoplasia and adrenal diseases.
“Part of our job of endocrinologists is the education of patients, but another important part is the education of other endocrinologists, and this presentation on ACC, a rare disorder that many endocrinologists are not very familiar with, is part of that,” Dr. Levine says. “Not every endocrinologist is near a major medical center, and often, there’s only one endocrinologist in a community. Sharing what we know is the right thing to do.”