The lack of definitive clinical evidence has made feminizing gender-affirming hormone therapy (GAHT) a less-than-precise science for endocrinologists who monitor and treat these individuals. Two 2024 studies from Mount Sinai—one on the risk of venous thromboembolism (VTE) in transgender people and the other on understanding the effects of estrogen dose and route of administration on serum levels—provide vital information and insights that clinicians can apply to their practice.
“These seminal studies are focused on closing the knowledge gap and advancing the field’s understanding and application of gender-affirming hormone therapy,” says Daniel Slack, MD, Assistant Professor of Medicine (Endocrinology, Diabetes and Bone Disease) at the Icahn School of Medicine at Mount Sinai, and first author of the two papers. “Both are quite provocative and will serve as additional tools for providers caring for patients using feminizing hormone therapy.”
Assessing Venous Thromboembolism
Few areas are of greater concern to those prescribing feminizing hormones to transgender people than the risk of VTE, given the potential for pulmonary embolism and stroke. Past studies, though limited in scale, have suggested that the potential of VTE in transfeminine individuals is increased compared to their cisgender counterparts.
Mount Sinai researchers painted a much different and more comprehensive picture in a retrospective analysis of 2,126 transfeminine and gender-diverse adults, detailed in a study published in November 2024 in Endocrine Practice. Above all, they found that 17 individuals, or 0.8 percent, had VTE. This prevalence, while higher than that observed in the general population, is lower than the 2 percent found in a previous meta-analysis that pooled studies of trans- and gender-diverse individuals. In addition, the Mount Sinai team found that VTE was driven not by any one risk factor, but by a combination of medical and nonmedical factors. Among the medical factors were already established links, including a genetic predisposition to blood clots and a history of high cholesterol, diabetes, and hypertension, all associated with poor cardiovascular health. Nonmedical factors, which researchers called “surrogate determinants of health,” included socio-economic status, race/ethnicity, and insurance status. Importantly, the use of exogenous estrogen was not found to be associated with an increased risk of VTE in the study population.
“Based on findings from our cohort, it’s reasonable to conclude that individuals who have experienced VTE tend to be more medically complex, as indicated by their older age and higher prevalence of comorbidities,” Dr. Slack says. “Conversely, younger patients without existing risk factors may have a relatively lower risk of VTE.”
The message for endocrinologists from this groundbreaking research is clear. “A patient’s risk for VTE must be evaluated in the context of their whole biopsychosocial experience, and not by putting a magnifying glass over just estrogen use,” Dr. Slack says. “In some cases, this could mean changing the dose or route of administration of estrogen. But it shouldn’t mean withholding gender-affirming hormone therapy from otherwise healthy individuals—a decision that could have a devastating impact on the patient, and be completely unnecessary.”
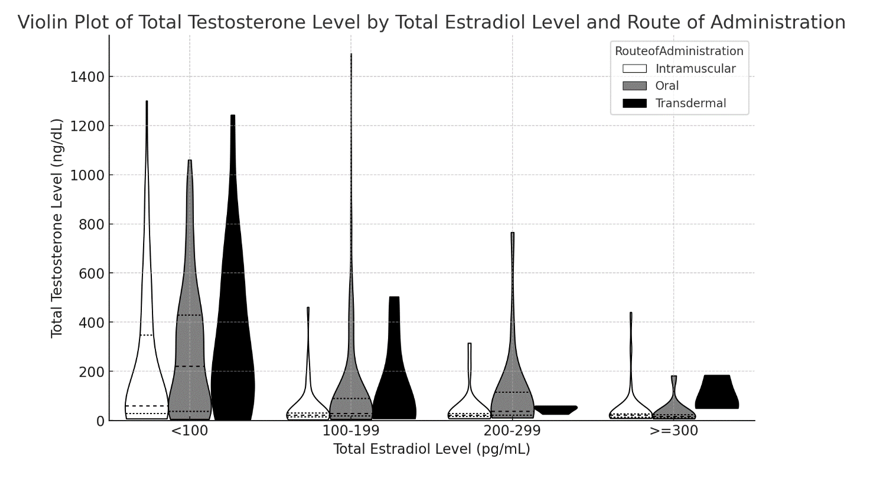
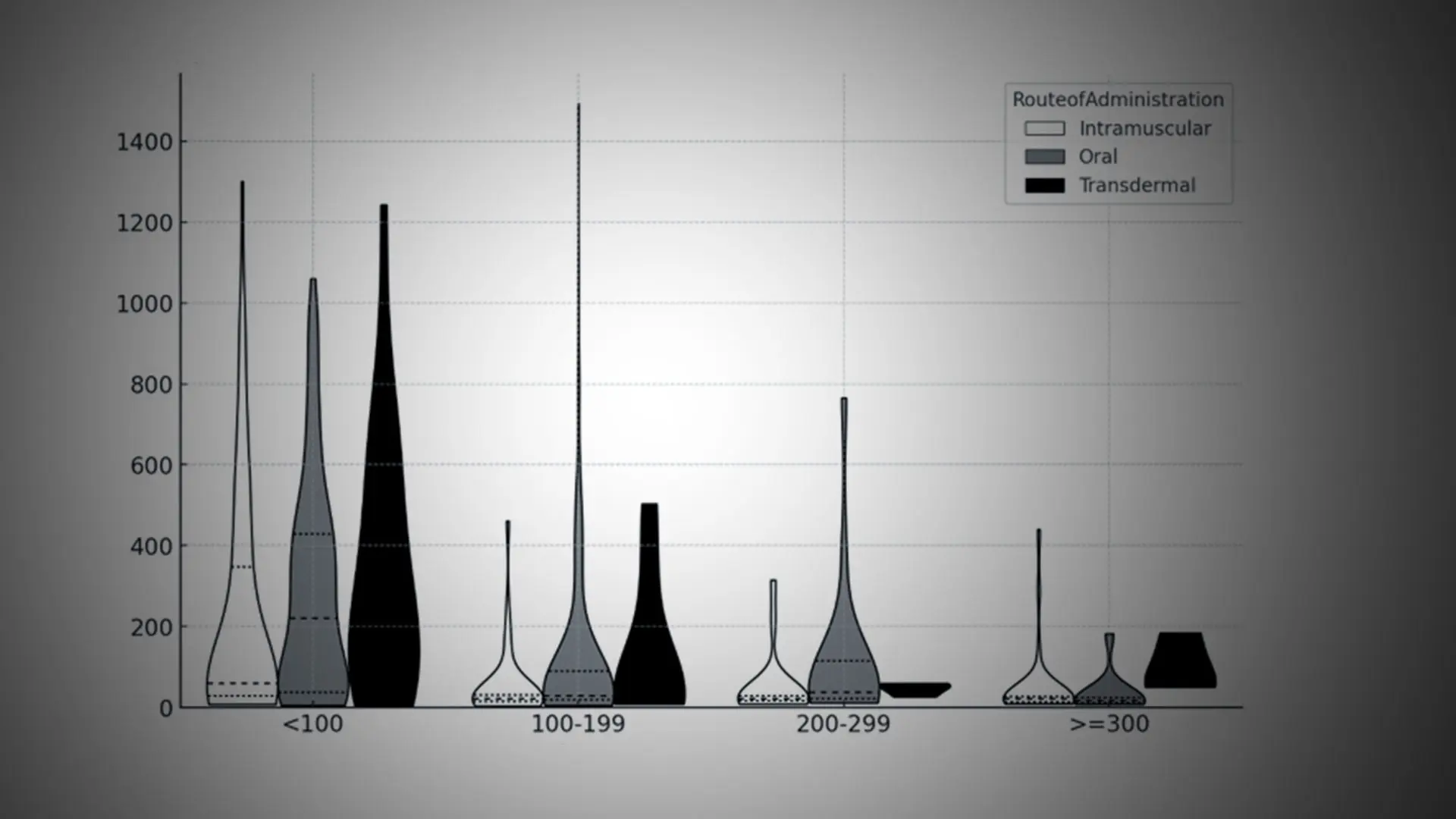
Total testosterone level by total estradiol level and route of administration in transfeminine GAHT.
“These seminal studies are focused on closing the knowledge gap and advancing the field’s understanding and application of gender-affirming hormone therapy.”
Daniel Slack, MD
Optimizing Dose and Route of Administration
For people seeking gender-affirming hormone therapy to align their physical appearance with their gender identity, the Endocrine Society and World Professional Association for Transgender Health (WPATH) recommend targets of serum testosterone levels below 50 ng/dL and serum estradiol levels between 100-200 pg/mL. However, there is little knowledge of what the precise impact of using a range of doses of estrogen (especially estradiol) and route of administration—including oral, intramuscular (IM), subcutaneous, transdermal, sublingual, and vaginal—will be on serum levels.
For the first time, Mount Sinai researchers gave the field precise evidence on which to base their sex hormone decisions for transfeminine patients, in a study published in October 2024 in Endocrinology Practice.
“We learned that intramuscular administration is the most potent form of administration compared to oral and transdermal routes,” says senior author Joshua Safer, MD, Professor of Medicine (Endocrinology, Diabetes and Bone Disease) at the Icahn School of Medicine at Mount Sinai and Executive Director of the Mount Sinai Center for Transgender Medicine and Surgery. “IM was associated with the highest levels of estradiol in the serum and the lowest levels of testosterone, which in many situations are the optimal goals.”
Another major finding of the study was that testosterone appears to be a more reliable biomarker for managing hormone therapy than estradiol—when the dose goes up, the testosterone level goes down. There was no such correlation with estradiol.
Dr. Safer says, “As clinicians, we obviously want to monitor serum levels in an informed and exact manner, and not arbitrarily adjust the dose to hit recommended guidelines without really knowing if it will achieve that outcome. In that regard, we learned testosterone appears to be a more dependable metric for measuring GAHT care.”
Featured

Joshua Safer, MD
Professor of Medicine (Endocrinology, Diabetes and Bone Disease); Director, Center for Transgender Medicine and Surgery

Daniel Slack, MD
Assistant Professor of Medicine (Endocrinology, Diabetes and Bone Disease)