Severe hypercortisolism due to ectopic adrenocorticotropin (ACTH) syndrome is a rare orphan disease, but this has not diminished its importance for Alice C. Levine, MD, Professor of Medicine (Endocrinology, Diabetes and Bone Disease) at the Icahn School of Medicine at Mount Sinai. A female patient with the disease who died of cardiac arrest just days after being transferred to her care over a decade ago has left an indelible imprint on her ever since.
“An autopsy found the culprit—a tiny benign tumor in the patient’s bronchus that was producing the ACTH that killed her,” recalls Dr. Levine. “Determining the source and treating these tumors is extremely difficult, especially when they’re benign, and I vowed at the time that no one should have to die again of severe hypercortisolism and its complications.” That concern has only grown in recent years as the number of these cases treated at the Mount Sinai Adrenal Center has increased dramatically, fueled in part by new therapies that have prolonged the life of individuals with neuroendocrine tumors.
Dr. Levine took a step to advance treatment of this disorder in December 2020. She convened a two-day virtual conference involving an interdisciplinary team of Mount Sinai experts in adrenal disorders and neuroendocrine tumors to create a clinical pathway for the medical and surgical management of Cushing syndrome resulting from ectopic production of ACTH. The goal: To make clinicians aware of the complications associated with extreme hypercortisolism and, more specifically, how to effectively address them.
The comprehensive recommendations that emerged from that conclave were outlined in May 2022 in the Journal of the Endocrine Society. They cover diagnosis, localization, surgical approaches to intrathoracic tumors and bilateral adrenalectomy, perioperative and postoperative medical management of hypercortisolism, and the appropriate selection and coordination of each of these critical components.
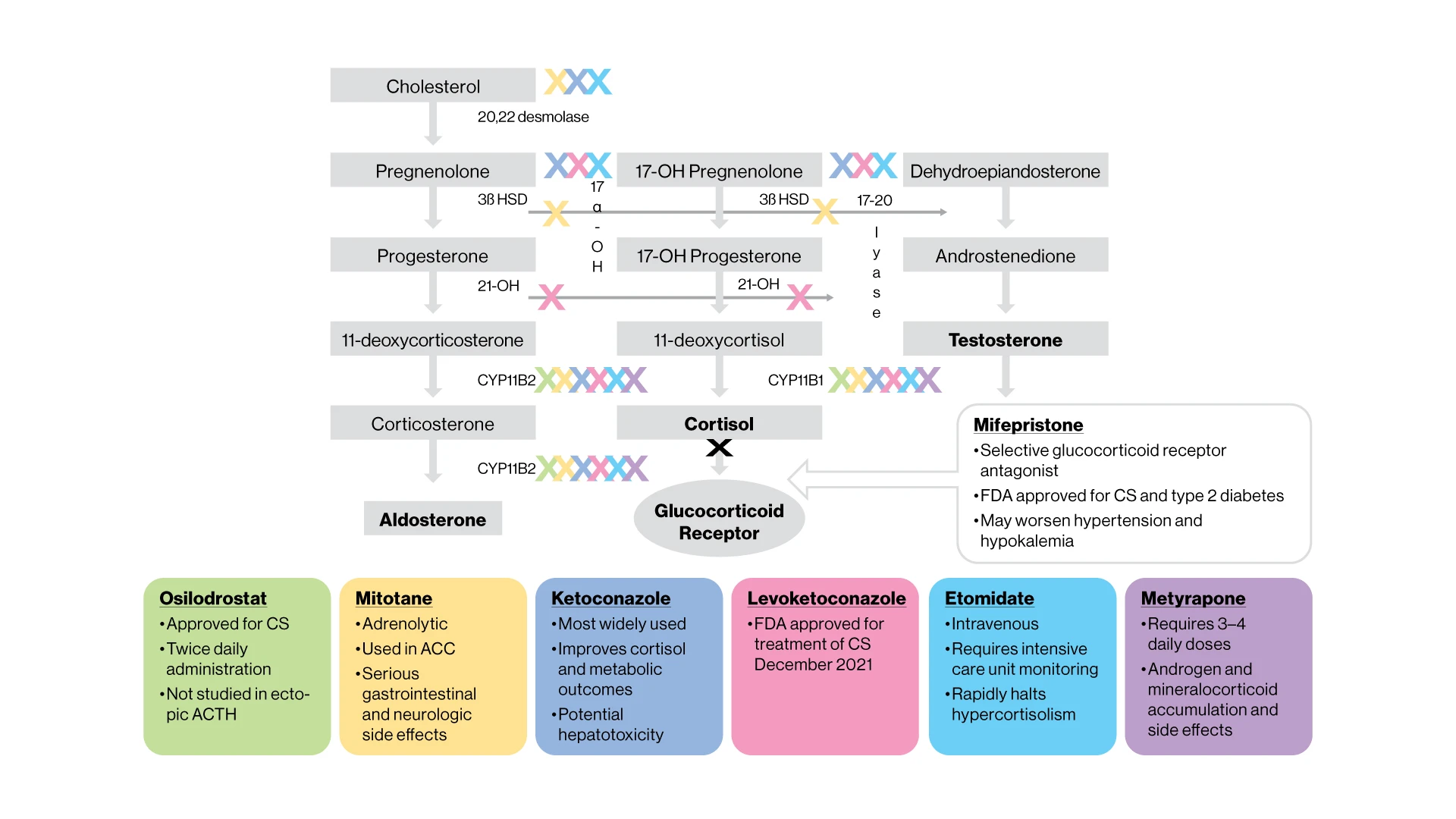
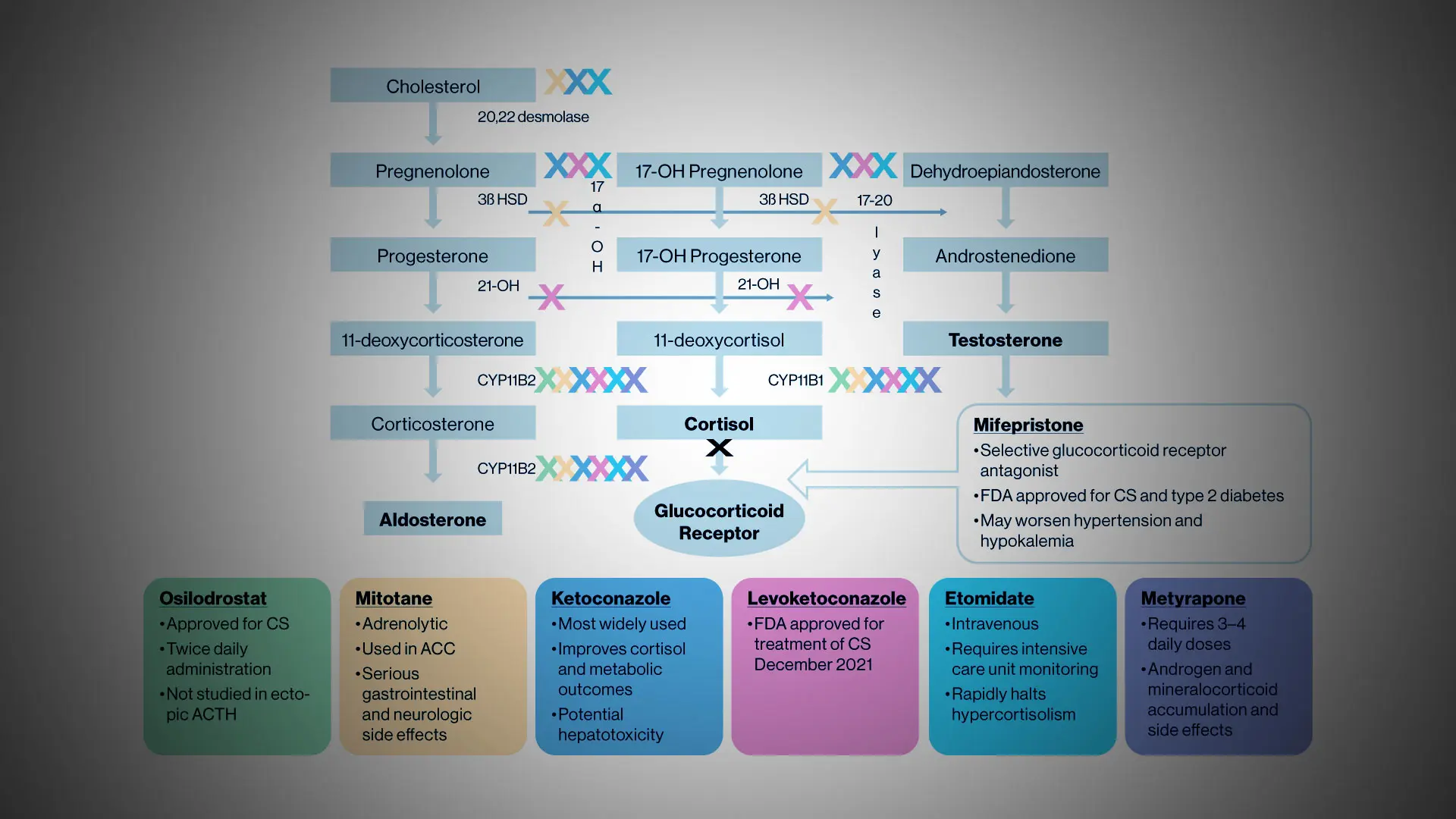
Cortisol synthesis inhibitors and receptor blockers. Sites of inhibition are demarcated by “X,” color matched to the boxes below with the corresponding drug
“Prior to our recommendations, we were handling patients with hypercortisolism on a case-by-case basis without any clear-cut guidance on who to send them to, what imaging and biochemical testing need to be obtained and in what order, which medications to administer, and when to refer the patient for surgery,” Dr. Levine explains. “Our pathway is really a blueprint for treating this life-threatening emergency in a coordinated and timely way through a team of endocrinologists, adrenal and thoracic surgeons, radiologists, anesthesiologists, and neuroendocrine oncologists at specialized centers.”
As for medical management, the guidelines recommend initial treatment with metyrapone, an off-label medicine on some hospital formularies (including Mount Sinai’s) that blocks cortisol synthesis and quickly lowers cortisol levels when administered in high and frequent doses. Ketoconazole or levoketoconazole may be added to the regimen if metyrapone alone is not effective; mifepristone should also be considered for acute and long-term management. Given the complexity of the disease, patients will likely require spironolactone, potassium supplementation, anticoagulation, diabetes control, and prophylaxis against the infection with trimethoprim-sulfamethoxazole.
If the hypercortisolism can’t be managed medically within several weeks, the protocols recommend bilateral adrenalectomy. While a laparoscopic approach is preferred, the decision should carefully weigh the patient’s surgical history and the experience and expertise of the surgeon.
Dr. Levine stresses that the clinical pathway developed by Mount Sinai can either be applied directly to patients with severe hypercortisolism, or used by tertiary care centers as a platform to develop their own procedures for the treatment and management of this endocrine emergency. “By identifying the scope of the problem along with appropriate diagnostic and therapeutic solutions, we believe we’ve performed a valuable service for the field,” she says. “We’ve already shown at our hospital that these protocols can truly make a difference in the lives of patients.”
Featured
Alice C. Levine, MD
Professor of Medicine (Endocrinology, Diabetes and Bone Disease)