A 61-year-old patient with cirrhosis and previously well-managed type 2 diabetes arrived at The Mount Sinai Hospital, gravely ill with diabetic ketoacidosis (DKA). The patient, who is an Emergency Medicine physician, had experienced several episodes of DKA over the past few months and had been treated at other area hospitals. His cirrhosis, which had been stable for more than 10 years, became acutely decompensated after the DKA episodes.
“I think the doctors kept assuming that maybe the patient wasn’t taking his insulin. But that wasn’t the case,” says a physician who led his successful treatment, Nirali Shah, MBBS, Associate Professor of Medicine (Endocrinology, Diabetes and Bone Disease) at the Icahn School of Medicine at Mount Sinai. “He was a physician and was taking his medication exactly as he should.”
In this unusual and complex case, the patient had developed insulin antibody (IA)-mediated insulin resistance (IR). Repeated episodes of DKA had compromised his liver function to the point that doctors were considering putting him on the list for a liver transplant.
Instead, a multidisciplinary team at Mount Sinai utilized a treatment approach using centrifugal plasmapheresis and the immunosuppressant mycophenolate mofetil (MMF) to suppress and remove insulin antibodies and help the patient achieve glycemic control, ultimately stabilizing his cirrhosis. The approach was described in American Association of Clinical Endocrinology Clinical Case Reports in September 2021.
When the patient came to Mount Sinai for treatment, his medical team had difficulty controlling his blood sugar level, and he required an unusually large intravenous infusion of more than 1,000 units of insulin a day. Suspecting the possibility of an autoimmune phenomenon against insulin, Dr. Shah uncovered that he had developed insulin antibodies, which were targeting the insulin in his body and preventing the insulin’s mechanism of action. So it took a high dosage of insulin to stabilize his glucose level.
“Typically, we treat antibody-mediated insulin resistance with high doses of immunosuppressants,” Dr. Shah says. “But these medications metabolize through the liver, and the patient’s cirrhosis precluded this option.”
Dr. Shah worked to devise a novel approach with a transplant and transfusion pathology team: Priya Grewal, MD, Professor of Medicine (Liver Disease) and Director of the Liver Clinic at The Mount Sinai Hospital; Ian Baine, MD, PhD, Assistant Professor of Pathology, Molecular and Cell Based Medicine, and Suzanne A. Arinsburg, DO, Associate Professor of Pathology, Molecular and Cell Based Medicine, and Director of the Blood Bank and Transfusion Medicine for the Mount Sinai Health System. Together, the team determined that centrifugal plasmapheresis would lower the antibody levels in his blood, they administered MMF to suppress the production of the antibodies that were causing the insulin resistance.
“Typically, we treat antibody-mediated insulin resistance with high doses of immunosuppressants. But these medications metabolize through the liver, and the patient’s cirrhosis precluded this option.”
Nirali Shah, MBBS
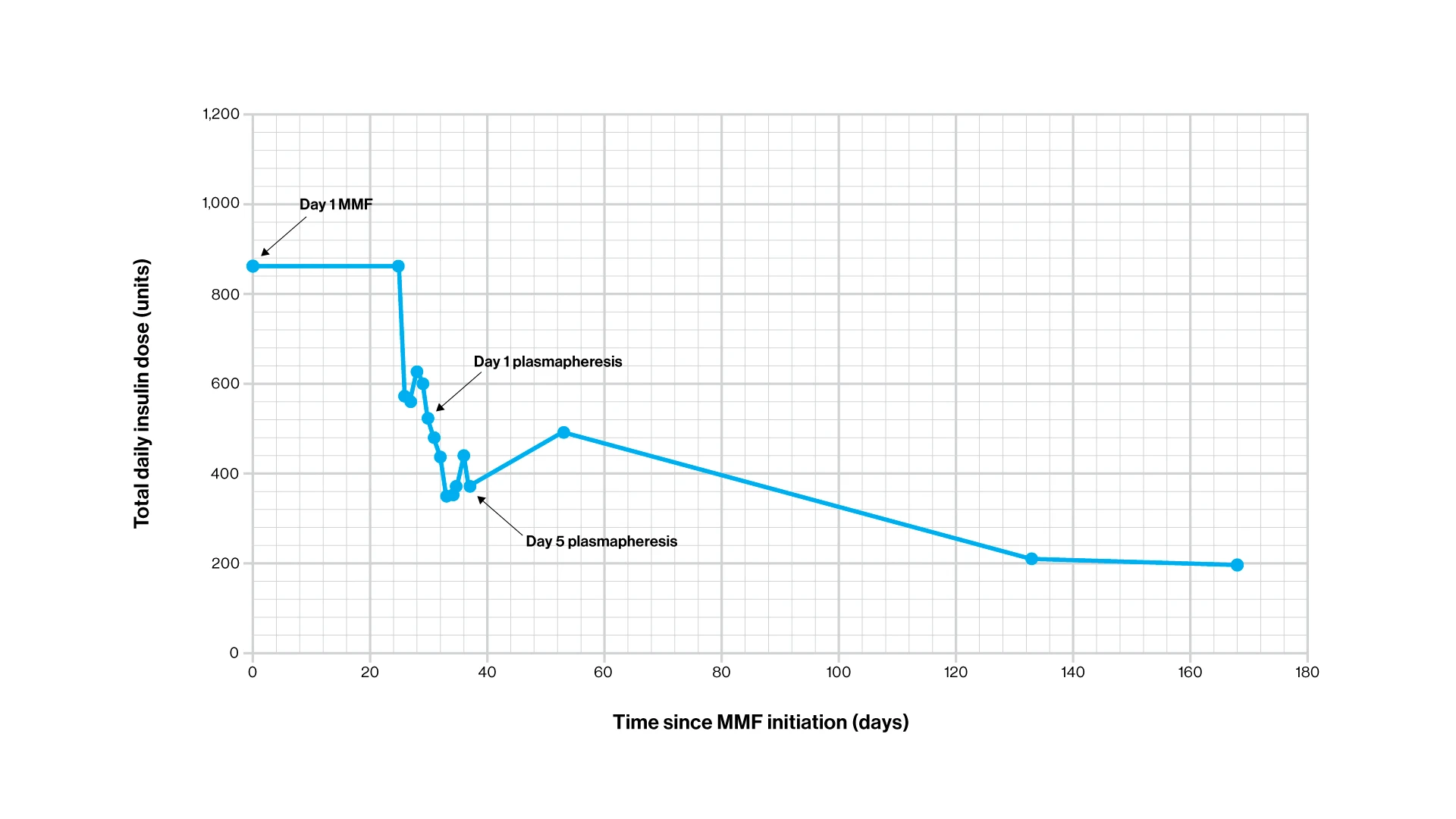
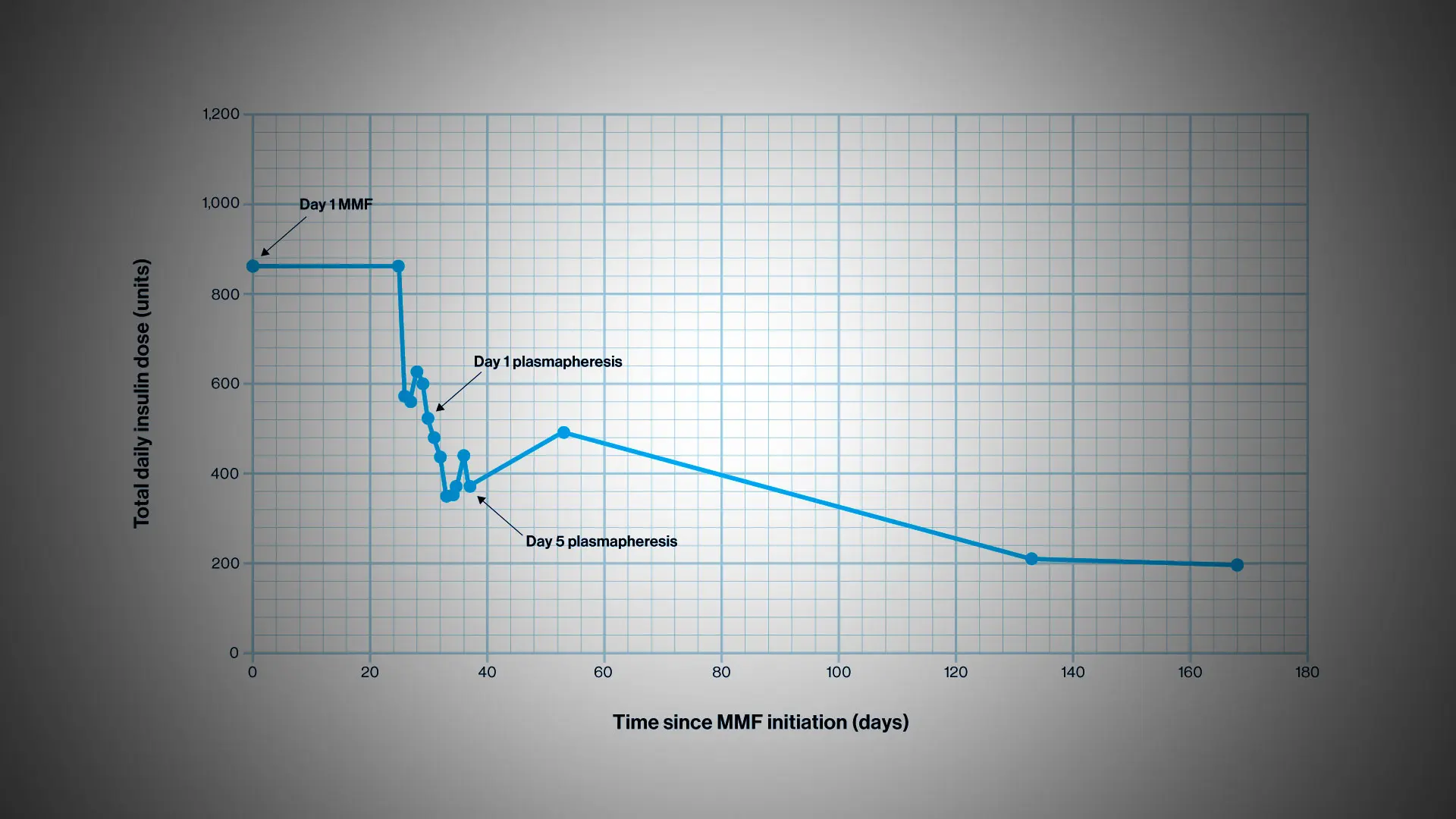
Graph showing the decrease in total daily insulin dose over time after mycophenolate mofetil (MMF) initiation. Further reduction in insulin requirement is demonstrated after plasmapheresis occurring on days 29 through 37.
The patient started MMF (500 mg twice daily), with improvement in finger-stick glucose testing in the range of 70-220 mg/dL. After one month of therapy with MMF, he was admitted to a monitored unit for a series of five plasmapheresis sessions. The patient was placed on an insulin drip with hourly glucose testing to allow for rapid insulin titration in the event of any hypoglycemia during antibody clearance. He was transitioned to glargine and U-500, the doses of which were reduced daily due to hypoglycemia.
He continued MMF throughout the plasmapheresis course, with dosing following each session, and continued MMF monotherapy post-discharge. Continuous glucose monitoring was utilized to monitor glycemic control pre- and post-therapy.
The approach proved successful. After one month of MMF, the patient’s total daily dose of insulin was reduced by 27.3 percent. After the five sessions of plasmapheresis, the insulin requirement fell an additional 29.7 percent (total reduction of 57 percent). Following an insulin regimen of 85 units U-500 with breakfast and lunch and 25 units of lispro with dinner for six months, the patient achieved an overall 77.3 percent decrease from his pretherapy insulin requirements.
Two years after this treatment, the patient needs 100 to 150 units of insulin a day, a 90 percent decrease. In addition, the patient has had no more episodes of DKA, and his liver disease stabilized, delaying the need for a liver transplant.
Various immunosuppressive regimens have been described to treat IA-mediated IR, yet there is no consensus on the optimal treatment for these patients, the report noted. The patient in this case highlights additional factors to consider when there is underlying cirrhosis, including increased infection risk. The approach using MMF and plasmapheresis to deplete IA may be a particularly effective method to improve hyperglycemia in patients with IA-mediated IR. It could help to achieve glycemic control without requiring the use of corticosteroids or multidrug immunosuppression, thereby avoiding any potential additive infection risk.
“This is the first report of MMF and centrifugal plasmapheresis use to mitigate the effects of IA-mediated IR in a patient with cirrhosis,” the report concluded. “We recommend further studies to determine the utility of this treatment to improve care for patients at high risk for IA-mediated IR.”
Featured

Nirali Shah, MD
Assistant Professor of Medicine (Endocrinolgy, Diabetes and Bone Disease)