Andrea Dunaif, MD, Chief of the Hilda and J. Lester Gabrilove Division of Endocrinology,
Diabetes and Bone Disease, Icahn School of Medicine at Mount Sinai, a world leader in the
study of disorders of metabolism and reproduction, is heading an international research
program supported by a National Institutes of Health grant with collaborators in England, the
Netherlands, and South Korea to determine whether the novel subtypes of polycystic ovary
syndrome (PCOS) her team recently discovered are present in regionally and ethnically diverse populations of women with PCOS.
Dr. Dunaif has summarized more than 20 years of genetic studies in a state-of-the-science
review article published in January 2022 in Endocrine Reviews. This article discusses, for non-
geneticists and clinicians, recent genomic advances into PCOS causal pathways that are “deconstructing” PCOS.
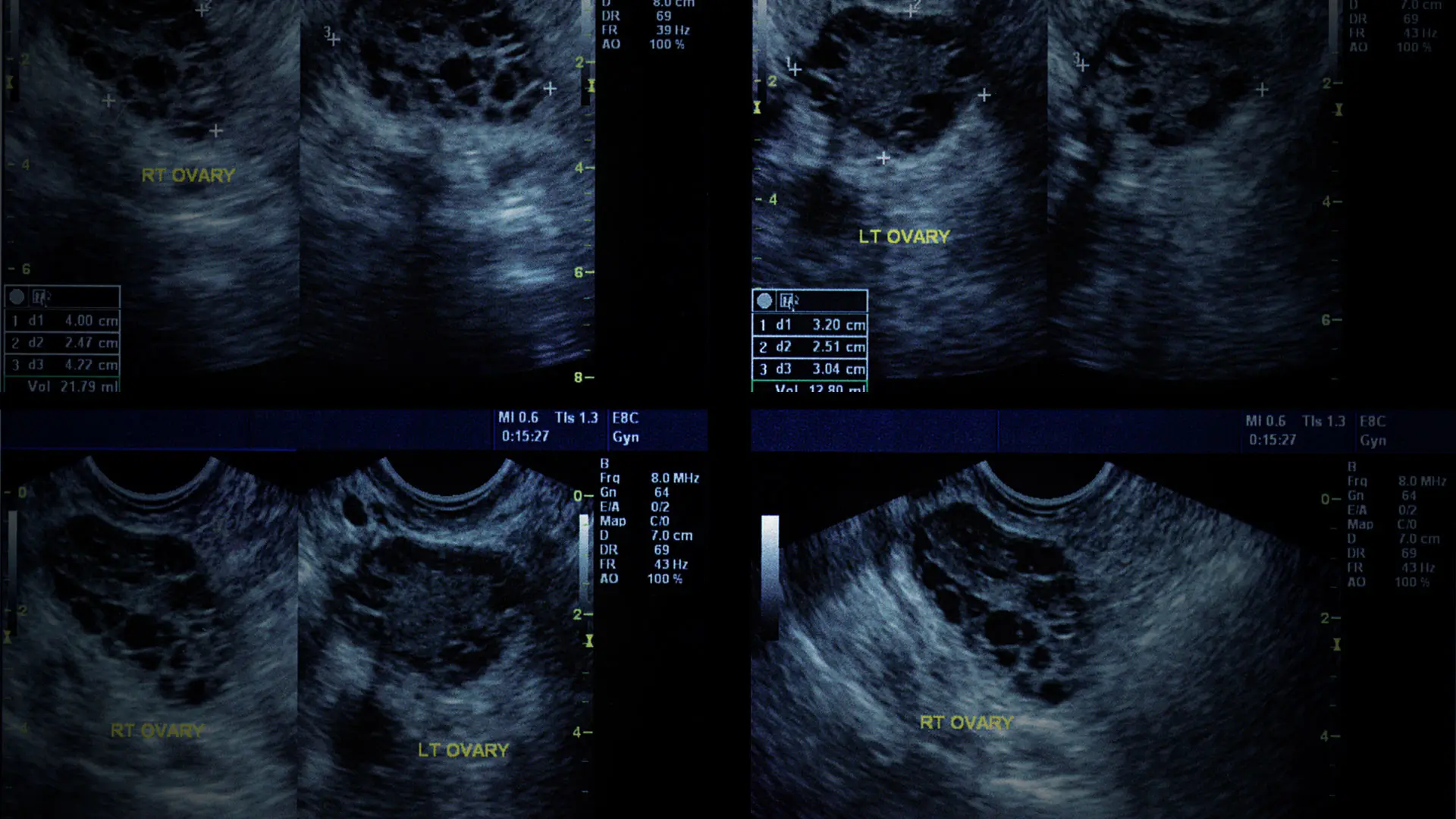
PCOS is among the most common disorders of women. It is characterized by clinical and/or
biochemical hyperandrogenism, oligomenorrhea, and polycystic ovarian morphology on
ultrasound (although the "cysts" are actually underdeveloped follicles). The condition is often
associated with insulin resistance and obesity, conferring increased risks for type 2 diabetes and cardiovascular disease.
Despite affecting up to 15 percent of reproductive-age women, PCOS remains poorly understood and under-diagnosed, says Dr. Dunaif, the Lillian and Henry M. Stratton Professor
of Molecular Medicine at Icahn Mount Sinai. And although it is widely recognized as a contributor to infertility, its long-term cardiometabolic health risks and reduced quality of life
for affected women are under-appreciated. Because its cause(s) is unknown, PCOS is currently
diagnosed using different sets of controversial clinical criteria based on expert opinion. Recent genetic analyses indicate that these diagnostic criteria do not identify biologically distinct PCOS subtypes.
Dr. Dunaif has published more than 150 papers on PCOS since the mid-1980s. Now, using
unbiased mathematical approaches combined with genetic analyses, she and her team have
recently escalated their efforts to biologically characterize the condition. In 2020, they
published findings in PLOS Medicine in which they identified biologically distinct “reproductive” and “metabolic” subtypes of PCOS using cluster analysis of clinical, hormonal, and metabolic features of the syndrome. These subtypes were associated with novel gene regions.
“PCOS can no longer be dismissed as a perplexing vicious cycle of hormonal disturbances. Its phenotypic and genetic heterogeneity clearly indicate the need to shift away from PCOS diagnosis based on expert opinion to criteria based on biologic mechanisms.”
- Andrea Dunaif, MD
Her group, along with international collaborators, has now identified these subtypes in women with PCOS of different ethnic groups. They intend to present and publish those results this year.
Dr. Dunaif notes the “omics” approaches are allowing the field to move from disease classification based on expert opinion, which is subjective, to classification based on demonstrable biologic differences. The impact of these biologic approaches is already evident in oncology, where cancer treatment is now based on molecular characteristics of tumors rather than their clinical presentation.
“Our study is one of the first demonstrations of the utility of this objective approach to the classification of a common disease, PCOS,” Dr. Dunaif says. “The resulting genetic knowledge promises to uncover the causes of PCOS and identify pathways to target for innovative PCOS therapies. The gene signals can also be used for testing to predict PCOS. The hormonal and genetic profiles of the PCOS subtypes can be used for personalized medical approaches to PCOS.”
Dr. Dunaif suggests that the name “PCOS” should be changed. “The name of this syndrome has nothing to do with what it really is. Now with subtypes, perhaps the scientific community will agree that nomenclature based on biologic mechanisms is more appropriate,” she says. “And in the long term, if we can understand how these genes work, then we can find different
pathways for drug targeting. Let’s say we find a gene that when activated causes part of PCOS. We could then develop an antibody to block it. I think that’s a plausible scenario, and very exciting.”
In the Endocrine Reviews article, Dr. Dunaif and co-author Matthew Dapas, PhD, now a
postdoctoral fellow in genetics at the University of Chicago and first author of the PLOS
Medicine article reporting the PCOS subtypes, summarize evidence for a genetic contribution to PCOS, and include a section “genetics for non-geneticists.” The review also covers PCOS
genetics pre- and post-GWAS, phenome-wide association studies, next-generation sequencing, the genetic architecture of PCOS including NIH, Rotterdam and novel subtypes, and environmental contributors including obesity, developmental origins, and epigenetic
inheritance.
The authors conclude, “PCOS can no longer be dismissed as a perplexing vicious cycle of
hormonal disturbances. Its phenotypic and genetic heterogeneity clearly indicate the need to
shift away from PCOS diagnosis based on expert opinion to criteria based on biologic mechanisms. By deconstructing the syndrome into its core components, genomics is leading
the transition toward precision medicine for PCOS. Affected women and their families, who
have been woefully underserved by the medical community, may at last look forward to
reaping the benefits of precision medicine in predicting, treating, and preventing PCOS.”
Featured

Andrea Dunaif, MD
Lillian and Henry M. Stratton Professor of Molecular Medicine; Chief of the Hilda and J. Lester Gabrilove Division of Endocrinology, Diabetes and Bone Disease