Related Article
Clinical trials are beginning on a new drug to treat kidney fibrosis—the culmination of more than a decade of work by John Cijiang He, MD, PhD, Chief of Nephrology at Mount Sinai Health System, and his team.
The journey began with the discovery by Dr. He’s laboratory of a specific regulator of kidney fibrosis called homeodomain interacting protein kinase 2 (HIPK2). Researching further, they recently identified an allosteric small molecule of HIPK2 which several animal models of kidney disease have shown is an effective anti-fibrosis drug. Preclinical testing has yielded encouraging results.
It is a classic example of dogged scientific determination, in which an interesting finding leads eventually to a significant advance, but not without a side trip or two along the way.
Dr. He, Irene and Dr. Arthur M. Fishberg Professor of Medicine at the Icahn School of Medicine at Mount Sinai, is an advocate of a systems biology approach to research, focusing on computational biology and bioinformatics to elucidate a fuller picture of interactions within an organism. By doing this, he strives to identify key drivers of disease processes, which could be potential drug targets for kidney disease therapy.
One focus of his research has been kidney fibrosis, a key element of the progression of chronic kidney disease. In a paper published in 2012 in Nature Medicine, Dr. He and colleagues, performing transcriptomic and proteomic studies of glomerular cells, found protein kinases that regulate gene expression in the kidneys of animal models with kidney fibrosis. The research team was able to identify HIPK2, the regulator of kidney fibrosis, and found that HIPK2 was upregulated in human kidneys with various types of kidney disease.
These findings were promising, since HIPK2 had never been identified as being important in the pathogenesis of kidney fibrosis. Clearly, this protein kinase had become a possible target for therapeutic intervention in kidney disease.
But there was a problem. Inhibiting all HIPK2-regulated pathways posed unwanted side effects. One downstream molecule, known as p53, could incite tumor growth if dysregulated by HIPK2. “If you inhibit HIPK2 you also inhibit p53,” Dr. He explains. “And because of that, there is a chance of developing cancer. That fact explains why several companies that were very interested in an anti-fibrosis drug walked away, their enthusiasm greatly reduced.”
An Important New Compound
Five years after their original study was published, Dr. He and his research team announced in the Journal of the American Society of Nephrology that they had identified BT173, which can specifically inhibit the TGF-β1/Smad3 pathway—an important pro-fibrotic channel—without also significantly inhibiting HIPK2 kinase activity or p53 activation. That finding made it possible to attenuate the renal fibrosis of chronic kidney disease (CKD) without employing the broad approach of inhibiting all HIPK2 pathways.
“This is a new compound,” Dr. He says. “It has a high potency and can be given as a PO dose daily instead of by IV injection.” TGF-β1 is thought to be the most important profibrotic element in kidney disease, and knockout of Smad3, a downstream target of HIPK2, has been found to reduce kidney fibrosis in animal models. Thus, blocking this pathway should be an effective approach to treating kidney fibrosis. “Our inhibitor blocks specifically the Smad3 activation,” Dr. He says.
A 2020 study in JCI Insight continued this work, further elucidating the novel mechanisms behind the anti-fibrosis role of HIPK2 in kidney disease. “This study will help develop better HIPK2 inhibitors for kidney disease,” Dr. He says.
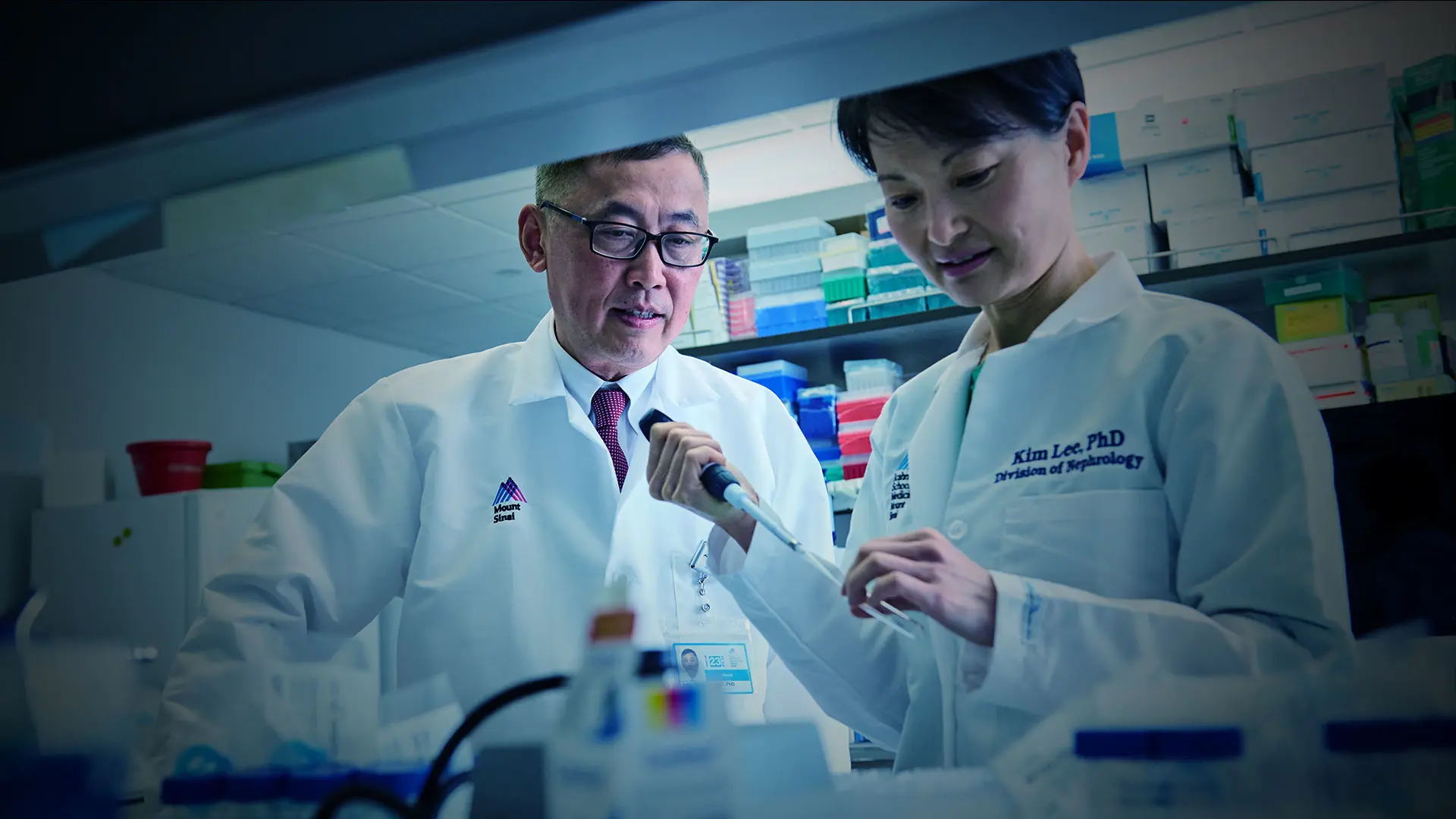
Cijiang He, MD, PhD, and Kyung Lee, PhD, are among the researchers working to develop and bring to market anti-fibrotic therapies.
Now, Dr. He and others, including Kyung Lee, PhD, Associate Professor of Medicine (Nephrology) at Icahn Mount Sinai, in collaboration with ShangPharma Innovation, Inc., have founded Rila Therapeutics, whose goal is to develop and bring to market anti-fibrotic therapies. Their focus will be on a small molecule developed from BT173. “Preclinical data have been very positive,” Dr. He says, adding they have so far seen no toxicity.
Clinical trials are expected to start in the spring of 2024. “This has been a really big journey, a 10-year story, but I think in the end a successful one,” says Dr. He.
The Division Is a Center for Research
Although Dr. He’s research is exciting, he is also quick to point out the impressive research being undertaken by his colleagues in the Division of Nephrology. The division has 20 National Institutes of Health (NIH)-funded Principal Investigators and receives about $15 million in NIH funding yearly—“one of the best-funded nephrology divisions in the country,” Dr. He notes.
The Mount Sinai division maintains both a registry of patients with CKD that numbers more than 150,000 and the BioMe Biobank with more than 10,000 specimens from patients with CKD—all vital elements of nephrology research. There is also a kidney tissue biobank that adds another 100 samples annually.
Mount Sinai’s nephrology research generates more than 100 high-impact papers in any given year, and investigators regularly engage in pharmaceutical company-sponsored randomized controlled trials. Licensing agreements with pharma companies and the generation of patents are ongoing.
Mount Sinai and Mount Sinai faculty members (Dr. He and Dr. Lee) have equity in Rila Therapeutics.
Featured Faculty and Division Leadership

Kyung Lee, PhD
Associate Professor of Medicine (Nephrology)

John Cijiang He, MD, PhD
Irene and Dr. Arthur M. Fishberg Professor of Medicine; Chief, Division of Nephrology