In the early days of the pandemic, some of the greatest uncertainties loomed over patients with inflammatory bowel disease (IBD) who wanted reassurance that their medications did not increase the risk of infection.
“We knew that steroids and other immunosuppressives used to treat IBD were associated with other infections, but we didn’t know if the same was true for COVID-19,” says Ryan Ungaro, MD, Assistant Professor of Medicine (Gastroenterology) at the Icahn School of Medicine at Mount Sinai. “We needed accurate, updated information fast so we could provide guidance to physicians and their patients about the safety of continuing their therapeutic regimens.”
That urgent need led to creation of an international registry, led by Mount Sinai in partnership with the University of North Carolina, to capture raw data from physicians about outcomes of IBD patients infected by SARS-CoV-2, the virus that causes COVID-19. Remarkably, that research database, known as SECURE-IBD (Surveillance Epidemiology of Coronavirus Under Research Exclusion), was developed within a period of weeks, a task that can typically take years. It immediately began meeting its goal: providing a quick and robust source of information to clinicians around the world about the use of IBD therapies like corticosteroids and the widely prescribed tumor necrosis factor (TNF) antagonists during the pandemic.
“Our data provided reassurance to patients and doctors that the vast majority of medications they were using for IBD were low-risk for COVID-19 outcomes,” reports Dr. Ungaro. “And that allowed them to feel more comfortable continuing or starting medications needed to keep IBD under control.”
"Steroids should be avoided as much as possible, and patients already on them should be tapered off as rapidly as possible."
Ryan Ungaro, MD
In a study based on data from SECURE-IBD, Dr. Ungaro and Jean-Frederic Colombel, MD, Professor of Medicine (Gastroenterology), found that systemic corticosteroids posed the highest risk for IBD patients with severe COVID-19, and that TNF antagonist therapy was not associated with adverse COVID-19 outcomes. “These findings reinforced that steroids should be avoided as much as possible, and patients already on them should be tapered off as rapidly as possible,” says Dr. Ungaro. “We were also able to suggest that biologics like TNF antagonist therapy appeared to be low-risk, relative to COVID-19, and that patients should continue to use them. In fact, our study showed that biologics might even protect against bad outcomes from the virus.”
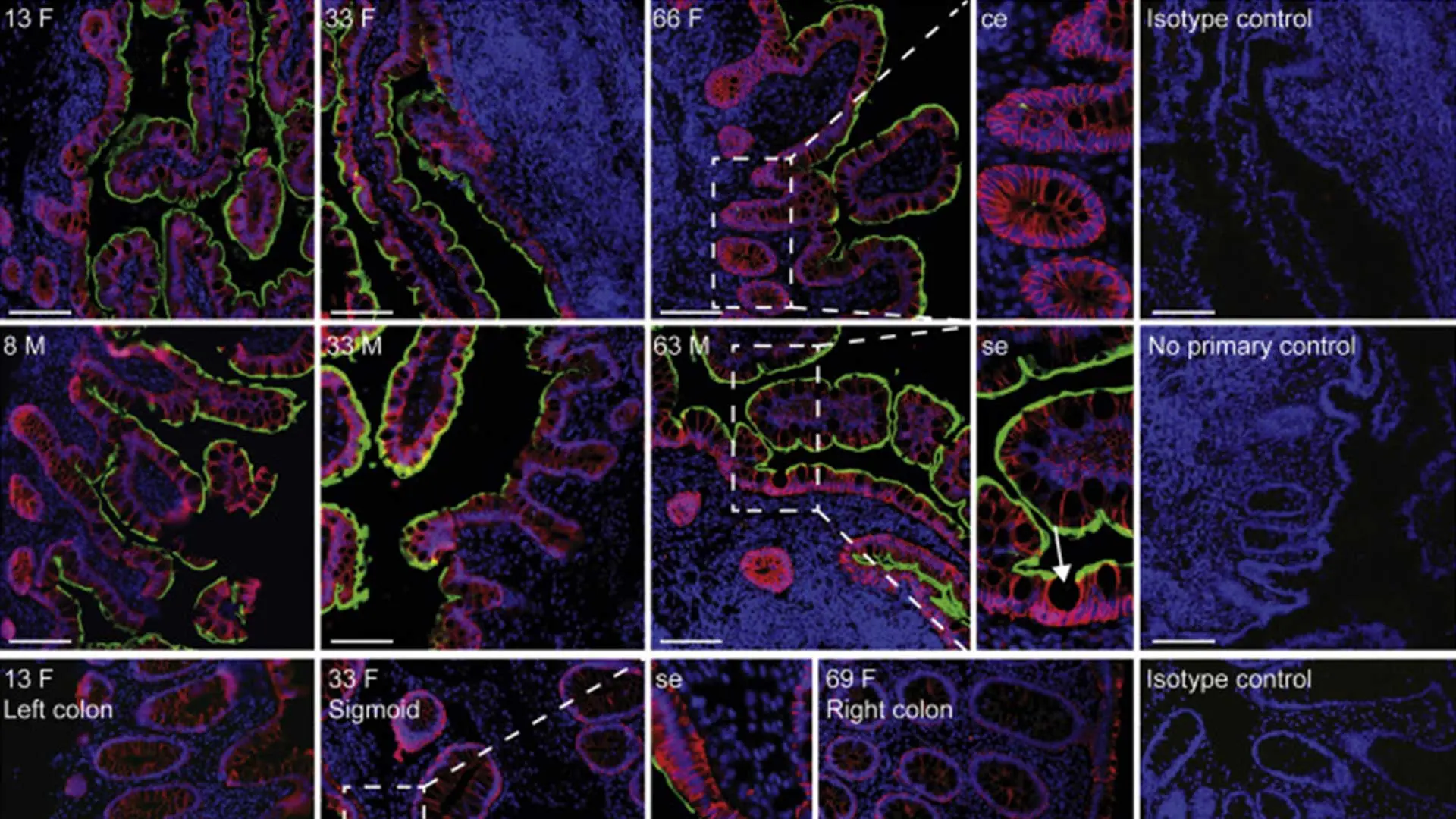
The effort to enhance awareness and guidance for the field around COVID-19 picked up steam in other ways at the Department of Medicine. “When the pandemic hit, my lab rapidly pivoted to understanding the mechanisms of COVID-19 in the GI tract,” says Saurabh Mehandru, MD, Associate Professor of Medicine (Gastroenterology). The focus was on angiotensin-converting enzyme 2 (ACE2) and transmembrane protein serine 2 (TMPRSS2). “We know that SARS-CoV-2 has a spike protein that tethers itself to ACE2 and that TMPRSS2 cleaves ACE2, enabling the virus to enter the host cell and replicate,” he explains. “The fact that the intestinal tract has the highest expression of ACE2 in the body—higher than even in the lungs—and that COVID-19 patients were presenting with symptoms like diarrhea, nausea, and vomiting, suggested to us gastrointestinal involvement in the disease progression.”
In their study, published in Gastroenterology, the researchers reported that while ACE2 is expressed in the respiratory system and the main cause of COVID-19-related mortality has been respiratory failure, the intestines also show robust expression of ACE2 and are highly susceptible to SARS-CoV-2. “We showed for the first time that this phenomenon is not occurring because there is a higher expression of ACE2 in the lungs, but because the lungs bear the brunt of the damage from the virus,” notes Dr. Mehandru.
The study also broke fresh ground by exploring the impact of biologic and non-biologic IBD therapies on ACE2 and TMPRSS2. “Since inflammation seems to drive receptor expression, we found no harm in patients continuing to receive IBD treatment when required,” Dr. Mehandru says. “Treating inflammation could actually result in better outcomes since it prevents hospitalization that might expose patients to the virus, and because immunosuppressive agents could block the overreaction of the immune system that has been linked to COVID severity and mortality.”
Featured
Jean-Frederic Colombel, MD
Professor of Medicine (Gastroenterology)

Bruce E. Sands, MD, MS
Dr. Burrill B. Crohn Professor of Medicine; Chief, Dr. Henry D. Janowitz Division of Gastroenterology