
Brian Abittan, MD, specializes in new hair rejuvenation techniques as well as continuing to improve ways to tighten and rejuvenate the skin.
Having built a national reputation for cutting-edge clinical and bench research and identifying new therapies around inflammatory skin disease, the Kimberly and Eric J. Waldman Department of Dermatology at the Icahn School of Medicine at Mount Sinai is now applying its vast trove of basic science and clinical expertise to the exciting and rapidly growing field of cosmetic dermatology. To that end, it is developing a comprehensive Center for Skin Aging to bring together its well-honed strengths in research, clinical trials, and the use of innovative procedures like lasers and radiofrequency microneedling to cosmetically treat and rejuvenate the maturing skin of patients.
“We want to revolutionize the approach to cosmetic dermatology the same way we’ve done for medical dermatology,” says Ahuva Cices, MD, Assistant Professor, Dermatology, at Icahn Mount Sinai, who is both a physician and scientist focused on cosmetic therapies for patients with autoimmune diseases. “In order to do that, we need to improve our understanding of what changes occur in normal healthy skin, and here we intend to rely on our basic science colleagues in the Department and the many innovative projects we have in development.”
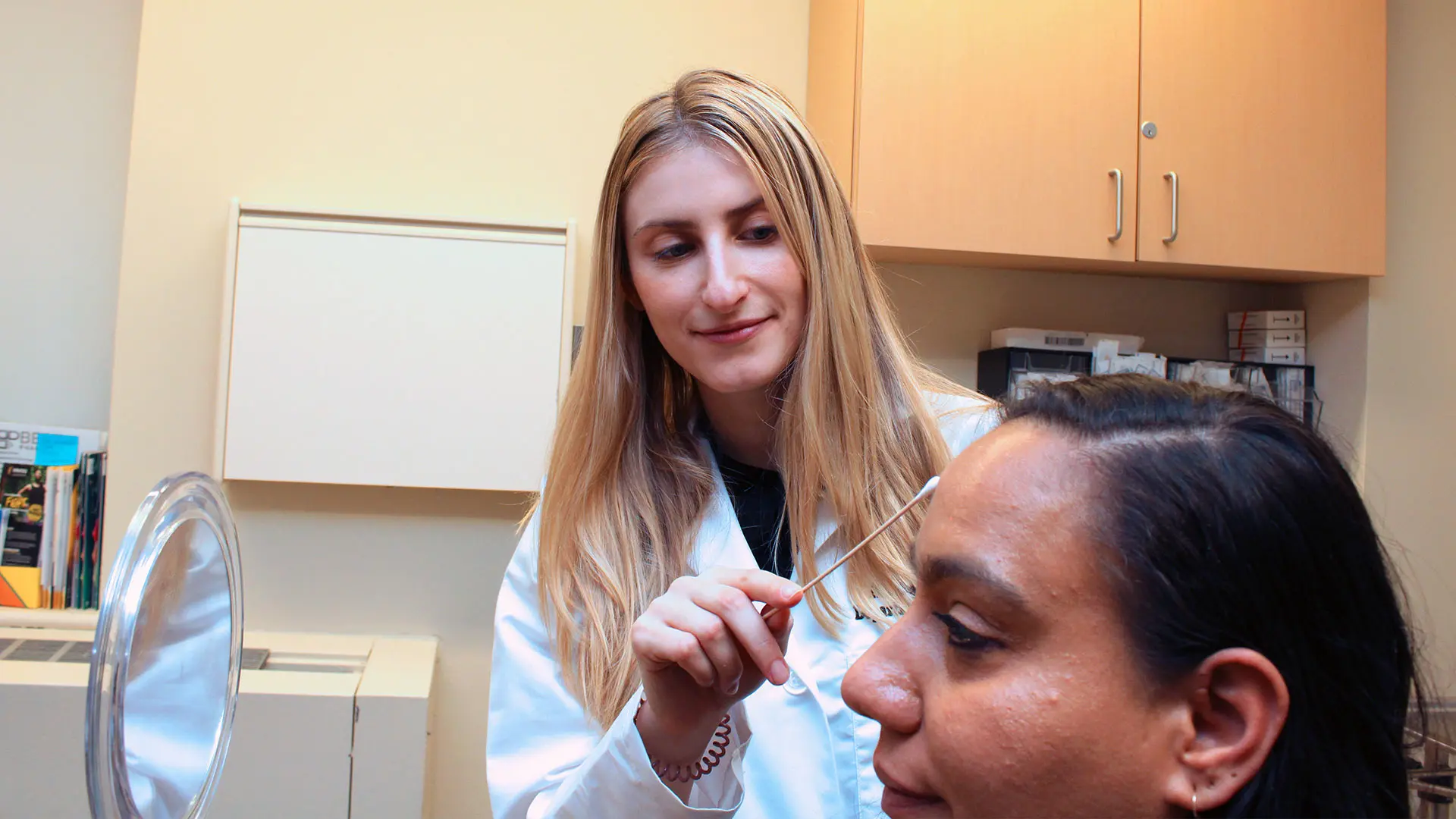
Ahuva Cices, MD, specializes in cutaneous manifestations of inflammatory bowel disease and cosmetic dermatology for patients with autoimmune disease, which serves the unmet needs of patients.
While cosmetic procedures targeting aging skin are commonplace today, what is noticeably absent is any linkage to clinical research. Mount Sinai’s dermatology team has a clear head start through its ongoing work at the cellular and molecular level with inflammatory skin disorders like atopic dermatitis, psoriasis, and alopecia areata. Among those researchers is Helen He, MD, a third-year dermatology resident who has already published many molecular and proteomic phenotyping studies on atopic dermatitis and other skin conditions, including the first cutaneous single-cell RNA sequencing profile of that disorder.
“We want to lend that same specificity to the study of skin aging to see if some of the inflammatory changes that occur in the immune system of people with atopic dermatitis, a disease considered by many to be a ‘human model of premature aging,’ are similar to the processes that take place with skin aging,” says Dr. He. “We hope to learn if some of the immunotherapeutics that we use in atopic dermatitis could also change the phenotype in non-disease individuals to improve their skin texture, integrity, and overall appearance. Only by knowing the mechanisms of skin aging can you find specific ways to target it.”
As a critical part of this unfolding research, Dr. He is profiling the maturation process of healthy skin by taking samples across the entire age spectrum, from young children to adults to the elderly. The goal is to uncover biomarkers that correlate well with age and could potentially serve as targets to reverse or modify in some way the skin aging process. In a meaningful break from past practice, investigators are collecting these samples coded with genetic and molecular data—including proteins, lipids, and the epidermal transcriptome—through the noninvasive or minimally invasive technique of skin tape stripping, which does not cause scarring or other morbidity, as do invasive approaches such as skin biopsies. This enables sampling from younger age groups and increases the ability to get larger numbers of samples needed for our increased understanding of aging processes.
We’ve been able in previous studies to capture the pathologic changes occurring in skin disease through tape strips with an accuracy that’s comparable to if not better than skin biopsies,” observes Dr. He. From this vital information collected both before and after cosmetic treatments, she hopes to get an unprecedented picture of the pathogenic changes occurring in the cutaneous landscape. “We will also couple these studies with blood studies aimed at understanding the ‘inflammaging,’ or inflammation associated with normal aging in healthy people as well as in the context of disease.”
One of those advanced treatments that dermatologists at Mount Sinai are already using—and looking to further improve in the lab—is the ellacor® laser procedure for skin tightening by removing micro-portions of excess or lax skin. This novel anti-aging technique for treating moderate to severe facial wrinkles, which is close to a facelift in its results, is available only at a few dermatology clinics across the United States and is unique in its ability to restore the skin’s structural integrity without invasive surgery and downtime for the patient. Moreover, the procedure is being carefully studied at Mount Sinai in combination with lasers, modulators, injectables, and energy-based techniques as part of research that would intensify under the planned Center for Skin Aging.
“Through research and advanced clinical practice, we continue to improve the ways to tighten and rejuvenate the skin by addressing each level and each layer with the most appropriate and least invasive treatment,” explains Brian Abittan, MD, Assistant Professor, Dermatology, at Icahn Mount Sinai, and Director of Skin and Hair Rejuvenation. “In addition, we’re able to customize facial tightening to all types of skin color, from darker to lighter. And the results we’ve seen in patients across these procedures is transformative.”

Angela J. Lamb, MD, offers the latest treatments, including minimally invasive cosmetic and laser procedures.
Dr. Abittan is further breaking ground for patients in the field of hair rejuvenation through the use of platelet-rich plasma (PRP), and in hair transplantation through a technique known as follicular unit extraction (FUE). PRP has become vital in hair restoration in the case of multiple forms of hair loss at Mount Sinai’s Alopecia Center of Excellence. This advanced technique draws a patient’s blood and spins it rapidly in a centrifuge, isolating the platelet-rich component from the rest of the blood. The content that remains is concentrated levels of a variety of naturally occurring growth factors. The PRP is then drawn into a syringe and injected into areas of the scalp where it’s needed to stimulate natural hair growth and, just as important, maintain it by slowing down further loss. FUE, for its part, eliminates the standard cut in the back of the scalp in favor of harvesting one follicle at a time and methodically implanting them in hair-deficient sections of the scalp. This method decreases recovery time and provides significantly better, more natural appearing results than the previous methods.
“Mount Sinai Dermatology offers comprehensive cosmetic, medical, and surgical interventions and clinical trials under one roof,” emphasizes Angela J. Lamb, MD, Vice Chair, Clinical Operations, and Associate Professor, Dermatology.
