Patients with long COVID may exhibit persistent inflammation in the heart and lungs for up to a year following SARS-CoV-2 infection, potentially placing them at elevated risk for future cardiac and pulmonary conditions. These findings come from a study conducted by researchers at the Icahn School of Medicine at Mount Sinai and published in April 2025 in the Journal of Nuclear Medicine.
The study, the largest of its kind using advanced PET/MRI imaging, discovered significant abnormalities in cardiovascular and pulmonary tissues, as well as altered levels of circulating immune-regulating proteins, in long COVID patients.
“Long COVID has emerged as a major public health challenge, and the long-term sequelae remain largely undefined,” says corresponding author Maria G. Trivieri, MD, PhD, Associate Professor of Medicine (Cardiology), and Diagnostic, Molecular and Interventional Radiology at the Icahn School of Medicine. “This study brings us closer to understanding how SARS-CoV-2 affects the heart and lungs over time. We believe long COVID results in an inflammatory response that may predispose patients to premature coronary artery disease, pulmonary hypertension, and valvular damage such as stenosis or regurgitation.”
“Since 2020, we have been publishing work showing that even mild or asymptomatic COVID infections can have serious cardiovascular consequences, even in previously fit and healthy individuals,” says David Putrino, PhD, the Nash Family Director of Mount Sinai’s Cohen Center for Recovery from Complex Chronic Illness. “This paper provides more data to highlight that SARS-CoV-2 is a virus that profoundly affects vascular health and that every new infection can do damage. Infection prevention is crucial.”
The objective of the study was to describe the prevalence of inflammatory cardiopulmonary findings in a prospective cohort of long COVID (LC) patients. Researchers recruited 98 adult Mount Sinai patients who had a confirmed COVID-19 infection between December 2020 and July 2021 and were experiencing persistent cardiopulmonary symptoms. Most of these patients had no previous diagnosis of cardiovascular disease. The most common LC symptom was shortness of breath (80 percent), and 27 percent of participants were hospitalized.
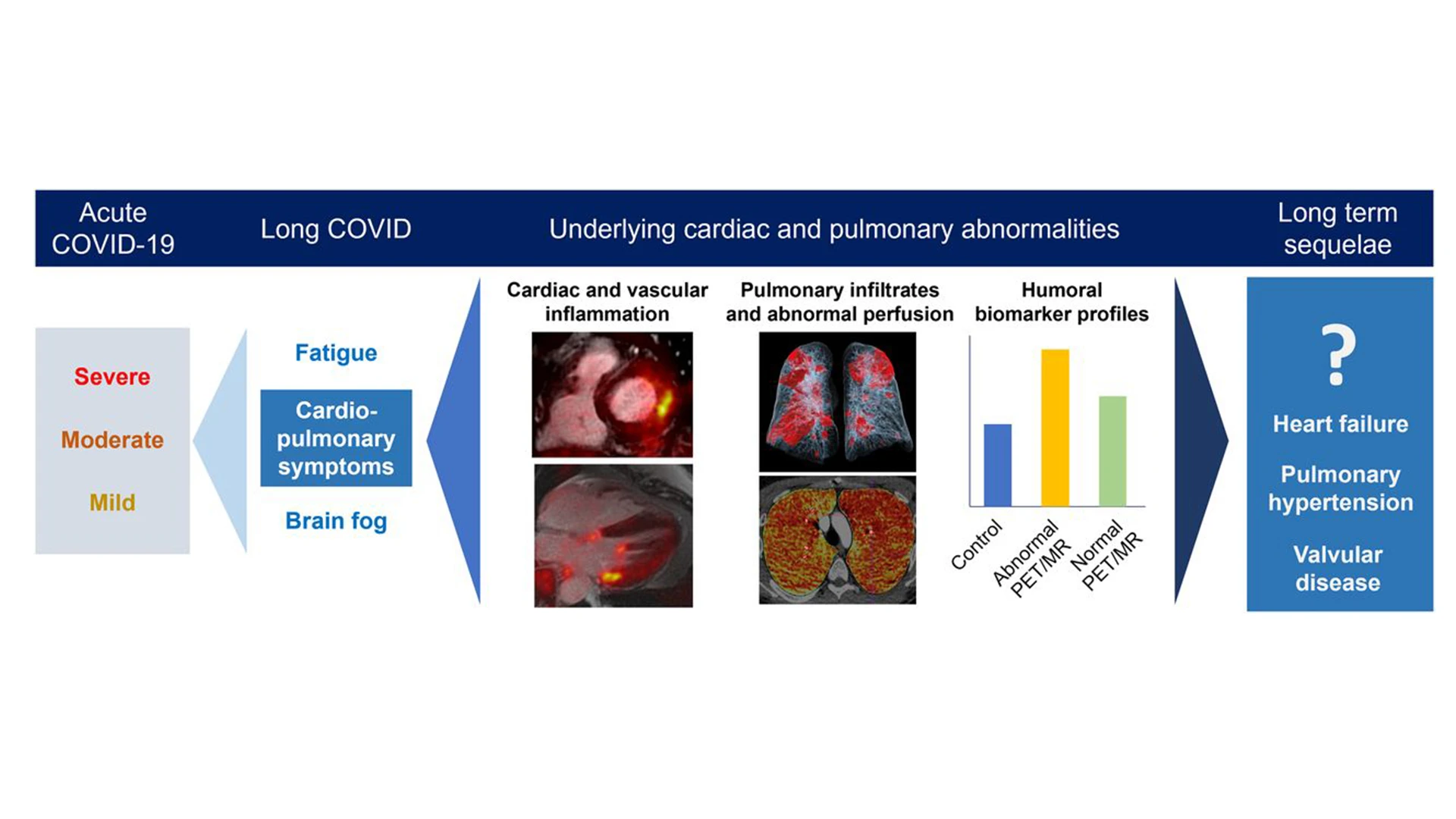
A graphic abstract of the study.
About 300 days after their initial infection, 91 participants underwent hybrid 18F-fluorodeoxyglucose positron emission tomography combined with magnetic resonance imaging (PET/MRI) and dual-energy CT (DECT) of the lungs. Among those scanned, 52 patients—57 percent—demonstrated evidence of inflammation affecting the heart muscle, pericardium, heart valves, particularly the mitral valve, and the aortic and pulmonary blood vessels. In several cases, more than one of these regions was affected. Of the subjects, 90 percent presented abnormalities in DECT, with 67 percent of participants demonstrating pulmonary infiltrates and 59 percent demonstrating abnormal perfusion.
The PET/MRI scans revealed myocardial abnormalities in 22 participants, characterized by scarring and thickening of the tissue, similar to findings of myocarditis or cardiomyopathy. Pericardial involvement was seen in 20 patients, indicating either inflammation or effusion. Inflammation near the mitral valve was identified in 10 participants, and vascular inflammation involving the aorta or pulmonary arteries was observed in 28 participants. All abnormalities were associated with persistent symptoms such as chest pain, fatigue, and shortness of breath.
In parallel, researchers performed plasma protein analysis, which showed abnormal patterns in key biomarkers that regulate inflammation and immune signaling. These findings correlated with the imaging abnormalities, providing molecular-level confirmation of persistent inflammation.
To further validate the results, a control group of nine individuals with confirmed prior COVID-19 infection but no lingering cardiopulmonary symptoms was studied between March and October 2023. These controls underwent the same imaging and blood testing and did not exhibit the inflammatory changes observed in the symptomatic long COVID cohort.
The study concluded, “In LC [long COVID] subjects evaluated up to a year after coronavirus 2019 infection, our results indicate a high prevalence of abnormalities on PET/MRI and DECT, as well as significant differences in the peripheral biomarker profile, which might warrant further monitoring to exclude the development of complications such as pulmonary hypertension and valvular disease.”
“We found a range of cardiopulmonary inflammatory patterns, backed by abnormal protein profiles,” Dr. Trivieri says. “These insights could have far-reaching implications for diagnosis and surveillance. If patients experience lingering symptoms such as shortness of breath, they should consult a physician for further evaluation. Our results should also raise awareness among clinicians to consider a patient’s COVID history and evaluate persistent symptoms more thoroughly.”
Zahi Fayad, PhD, senior author of the study and Director of the Biomedical Engineering and Imaging Institute at the Icahn School of Medicine, emphasized the broader impact of these findings. “This study highlights the unique power of hybrid PET/MRI imaging to uncover hidden disease processes in long COVID patients,” says Dr. Fayad, Professor of Radiology, and Medicine (Cardiology) at the Icahn School of Medicine and holder of the Lucy G. Moses Professorship in Medical Imaging and Bioengineering. “These findings should change how we approach care and surveillance—not only recognizing SARS-CoV-2 as a potential long-term cardiovascular risk factor, but also integrating molecular imaging into post-COVID evaluation protocols. We now have objective evidence that can guide earlier detection and potentially prevent future cardiopulmonary events.”
The Mount Sinai team continues to follow this patient cohort to assess long-term outcomes and is exploring whether these imaging and biomarker patterns can help predict who is most at risk for developing chronic cardiovascular or pulmonary disease after COVID-19.
Featured

Maria Giovanna Trivieri, MD, PhD
Associate Professor of Medicine (Cardiology), and Diagnostic, Molecular, and Interventional Radiology

David Putrino, PhD
Director of Rehabilitation Innovation, and Professor of Rehabilitation and Human Performance

Zahi Fayad, PhD
Lucy G. Moses Professor in Medical Imaging and Bioengineering, and Professor of Medicine (Cardiology)