Withdrawing aspirin one month after percutaneous coronary intervention (PCI) in high-risk heart patients and keeping them on ticagrelor alone safely improves outcomes and reduces major bleeding by more than half when compared to patients taking aspirin and ticagrelor combined (also known as dual antiplatelet therapy or DAPT), the current standard of care.
The breakthrough study, ULTIMATE-DAPT, was announced by Gregg W. Stone, MD, the study co-chair and Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai, during a late-breaking trial presentation at the American College of Cardiology Scientific Sessions in April 2024 and published in The Lancet.
“It is my belief that it’s time to change the guidelines and standard clinical practice such that we no longer treat most acute coronary artery syndrome (ACS) patients with dual antiplatelet therapy beyond one month after a successful PCI procedure,” Dr. Stone says. “Treating these high-risk patients with a single potent platelet inhibitor such as ticagrelor will improve prognosis.”
ULTIMATE-DAPT is the first and only trial to test high-risk patients with recent or threatened ACS taking ticagrelor with a placebo starting one month after PCI and compare them with ACS patients taking ticagrelor with aspirin over the same period. “Our study has demonstrated that withdrawing aspirin in patients with recent ACS one month after PCI is beneficial by reducing major and minor bleeding through one year by more than 50 percent,” Dr. Stone says. “Moreover, there was no increase in adverse ischemic events, meaning continuing aspirin was causing harm without providing any benefit.”
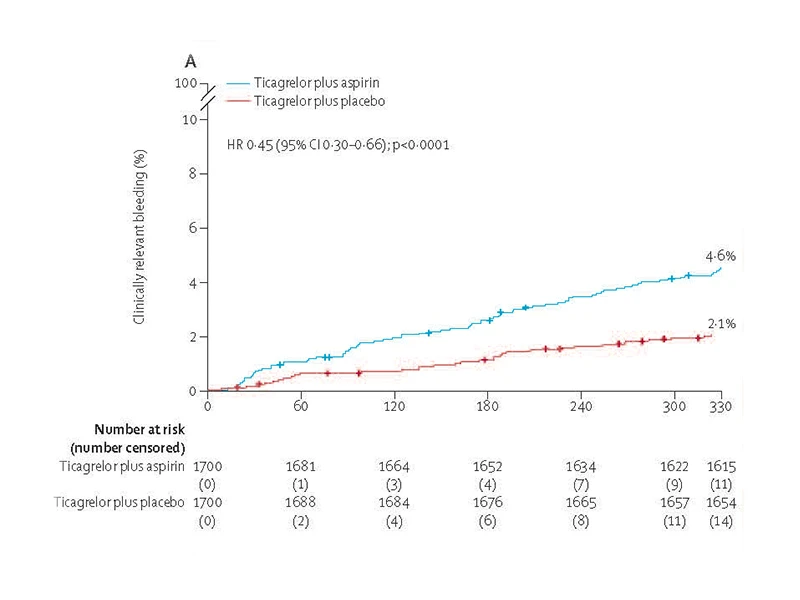
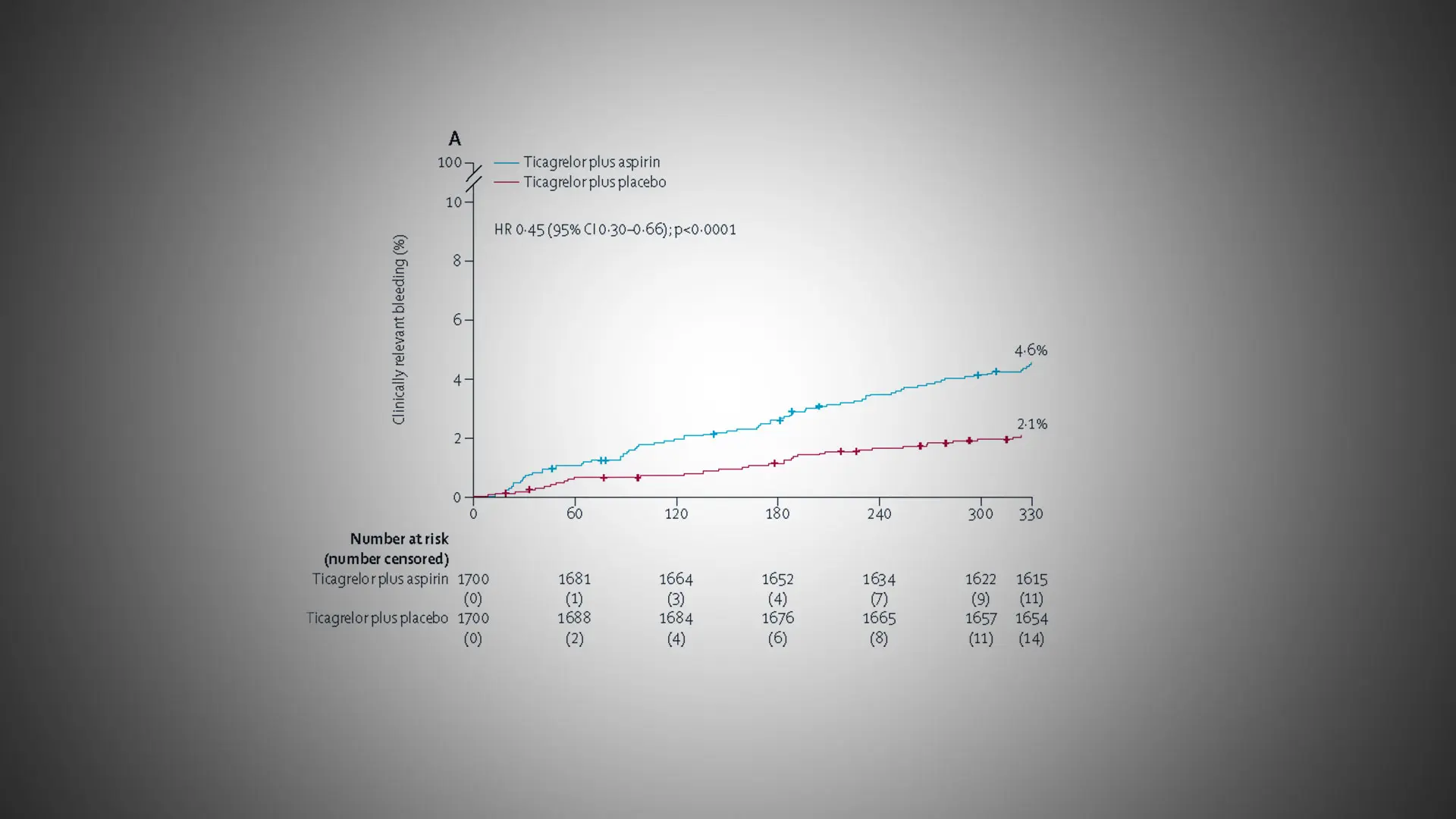
The primary efficacy endpoint of clinically-relevant bleeding, defined as BARC types 2, 3 or 5 bleeding, was assessed in the intention-to-treat population between one month and 12 months post-PCI in patients who were event-free after one month of ticagrelor and aspirin. Switching to ticagrelor monotherapy at one month resulted in a 55 percent reduction in the hazard of clinically relevant bleeding compared with continuing ticagrelor plus aspirin over the ensuing 11 months.
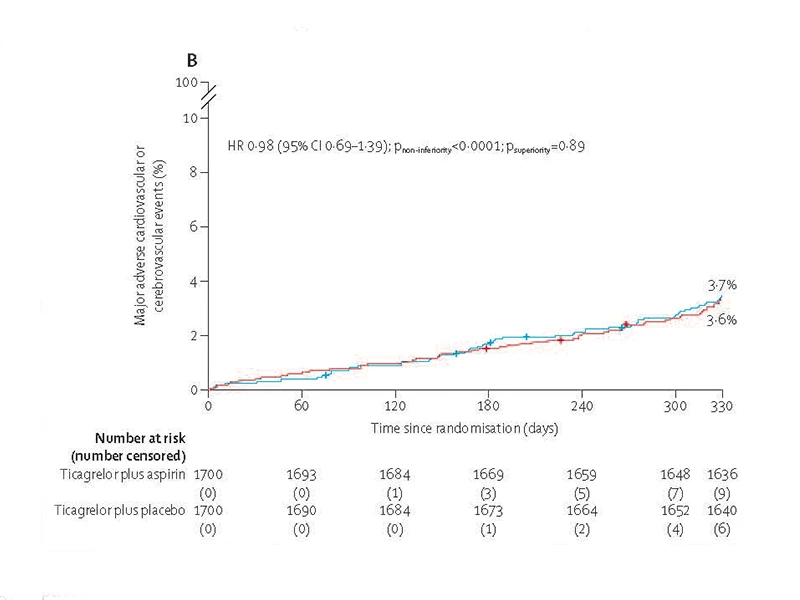
The primary safety endpoint of MACCE, the composite cardiac death, myocardial infarction, ischaemic stroke, definite stent thrombosis, or clinically-driven target vessel revascularization, was assessed in the intention-to-treat population between one month and 12 months post-PCI in patients who were event-free after one month of ticagrelor and aspirin. During the next eleven months, patients treated with ticagrelor monotherapy had similar rates of adverse ischemic events as patients who were maintained on ticagrelor plus aspirin.
The randomized, placebo-controlled, double-blind clinical trial analyzed 3,400 patients over age 18 with ACS at 58 centers in four countries between August 2019 and October 2022. All of the patients had undergone PCI. The patients were stable one month after PCI and were on ticagrelor and aspirin. Researchers randomized the patients after one month, withdrawing aspirin in 1,700 patients and putting them on ticagrelor and a placebo, while leaving the other 1,700 patients on ticagrelor and aspirin. All patients were evaluated between 1 and 12 months after the procedure. The two primary endpoints were MACCE (the composite of cardiac death, myocardial infarction, ischemic stroke, definite stent thrombosis, or clinically driven target vessel revascularization) and major or minor bleeding.
During the study period, 35 patients in the ticagrelor-placebo group had a major or minor bleeding event, compared to 78 patients in the ticagrelor-aspirin group, meaning that the incidence of overall bleeding incidents was reduced by 55 percent by withdrawing aspirin. MACCE events occurred in 61 patients in the ticagrelor-placebo group compared to 63 patients in the ticagrelor-aspirin group, a difference that was not statistically significant—further demonstrating that removing aspirin did no harm and improved outcomes.
“Along with the results from previous studies, these findings show that most patients in this population can benefit from aspirin discontinuation and maintenance on ticagrelor monotherapy after one month of dual antiplatelet therapy,” the study concluded.
“It was previously believed that discontinuing dual antiplatelet therapy within one year after PCI in patients with ACS would increase the risk of heart attack and other ischemic complications, but the present study shows that is not the case, likely because the current generation of drug-eluting stents have become so safe. Discontinuing aspirin in patients with a recent or threatened heart attack who are stable one month after PCI is safe and, by decreasing serious bleeding, improves outcomes,” Dr. Stone adds. “This study extends the results of prior work that showed similar results but without the quality of using a placebo, which eliminates bias from the study.”
This trial was funded by the Chinese Society of Cardiology, the National Natural Scientific Foundation of China, and Jiangsu Provincial and Nanjing Municipal Clinical Trial Project.
Featured
Gregg W. Stone, MD
Professor of Medicine (Cardiology), and Population Health Science and Policy