It is crucial to accurately estimate the severity of target lesion calcification during percutaneous coronary intervention (PCI) in order to define a treatment paradigm with the least risk for each patient. Mount Sinai researchers addressed this issue in two 2024 studies that describe a new approach for managing coronary calcium and calcified nodules with an evidence-based algorithm guided by optical coherence tomography (OCT) imaging.
“Our studies are among the first to compare multiple modification strategies specifically for calcified nodules using detailed OCT guidance,” says Annapoorna S. Kini, MD, Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai, and Director of the Samin K. Sharma Family Foundation Cardiac Catheterization Laboratory at The Mount Sinai Hospital. “This work further translates those modification strategies—which include rotational atherectomy, orbital atherectomy, and intravascular lithotripsy—into a practical, step-by-step treatment algorithm through intravascular imaging.”
One in five patients undergoing PCI will require plaque modification for calcified coronary lesions. These markers of atherosclerotic disease can complicate PCI by increasing the risk of suboptimal stent expansion as well as stent thrombosis and in-stent restenosis. Equally concerning for clinicians is the fact that coronary calcification is on the rise globally, propelled by an aging population and comorbid diseases such as diabetes mellitus and renal dysfunction.
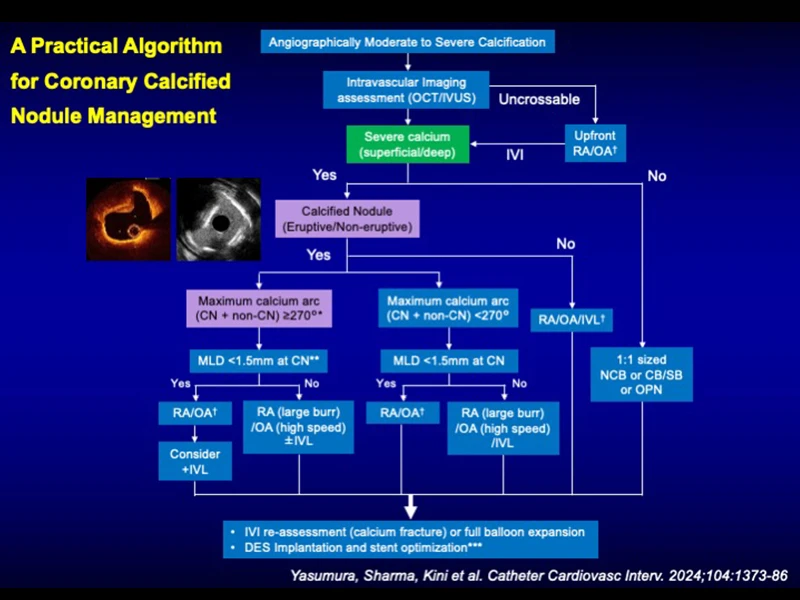
Notably lacking are comprehensive guidelines for the discernment of calcified nodules, whose morphological features have been associated with increased rates of target lesion failure following PCI. To address this issue, the team published studies in Catheterization & Cardiovascular Interventions in December 2024 and Progress in Cardiovascular Diseases in June 2024. The teams offer a treatment algorithm for individuals with moderate to severe calcification based on a retrospective analysis of patients undergoing OCT-guided PCI with calcium modification devices, including rotational atherectomy, orbital atherectomy, and intravascular lithotripsy.
“Our studies are among the first to compare multiple modification strategies specifically for calcified nodules using detailed OCT guidance.”
Annapoorna S. Kini, MD
A graphic abstract.
“The development of new technologies, most notably atherectomy devices, intravascular lithotripsy, and intravascular imaging, has changed the landscape of how we tackle coronary calcified lesions,” says Keisuke Yasumura, MD, co-author of the studies and Assistant Professor of Medicine (Cardiology), Icahn School of Medicine at Mount Sinai. “We found that integrating different calcium modification strategies based on lesion characteristics leads to more consistent procedural successes. This highlights the importance of tailored device selection and treatment approaches guided by intravascular imaging.”
The algorithm for managing coronary calcified nodules builds on these critical findings by suggesting upfront use of intravascular imaging assessment via OCT or intravascular ultrasound (IVUS) to evaluate the severity and morphology of the calcium. For severely stenotic or uncrossable lesions, it recommends use of rotational atherectomy or orbital atherectomy. As the study notes, “shaving” the protruding calcified nodule with RA or OA could reduce the risk of lesion re-protrusion through the deployed stent. On the other hand, “shaking” and fracturing the wide arc of the calcium sheet as well as modifying calcified nodules through intravascular lithotripsy can lead to optimal stent expansion.
“We’re hopeful that interventional cardiologists will adopt our proposed algorithm for managing coronary calcium and calcified nodules, recognizing the essential role of intravascular imaging for precise lesion assessment and individualized treatment,” says Dr. Kini. “Importantly, clinicians should not assume these techniques will be effective in the absence of advanced imaging guidance and appropriate patient selection.”
The Cardiac Catheterization Laboratory at The Mount Sinai Hospital is among the highest-volume and safest in the world, performing more than 15,000 procedures, including 5,200 interventions each year. For 15 years, the laboratory has hosted Complex Coronary Cases (CCC Live Cases)—a webcast that is viewed monthly by more than 10,000 physicians in 134 countries. During the webcasts, performed on the third Tuesday of each month, viewers are guided through a complex procedure by Dr. Kini, Samin K. Sharma, MD, Director of Interventional Cardiology for the Mount Sinai Health System, and the Anandi Lal Sharma Professor of Medicine (Cardiology), and Prakash Krishnan, MD, Director of Endovascular Interventions, and Professor of Medicine (Cardiology) and Diagnostic, Molecular and Interventional Radiology.
Participants are actively engaged and encouraged to ask questions during the webcast. “The overall goal of CCC Live Cases is to offer, to as many people as possible, unparalleled insight and training techniques in the complexities that physicians come across in the field of interventional cardiology,” Dr. Sharma says.
From CCC Live Cases: A 80-year-old male presented with new onset CCS Class I angina, negative limited stress myocardial perfusion imaging, but computed tomography angiography revealing a calcium score of 3173, three-vessel coronary artery disease and CT FFR+ in the left anterior descending artery and right coronary artery.
Featured

Annapoorna S. Kini, MD
Director of the Cardiac Catheterization Laboratory at The Mount Sinai Hospital, and the Zena and Michael A. Wiener Professor of Medicine
Samin K. Sharma, MD
Director of Interventional Cardiology, The Mount Sinai Hospital, and Anandi Lal Sharma Professor of Medicine in Cardiology