Researchers at the Icahn School of Medicine at Mount Sinai in September 2023 were awarded a $10.2 million grant from the National Heart, Lung and Blood Institute of the National Institutes of Health to investigate risk factors for malignant ventricular arrhythmias in mitral valve prolapse.
Of particular concern is the growing awareness of the connection between mitral valve prolapse and malignant arrhythmias—which can cause sudden death in a small but significant subset of patients. However, the early warning signs that might indicate the development of these life-threatening arrhythmias are not well understood.
“Since the initial descriptions of mitral valve prolapse syndrome, a linkage to the risk of sudden death was identified. Our recent work, along with that of others, is starting to unravel the connection between mitral valve prolapse and sudden death, as well as the changes that create the substrate for life-threatening ventricular arrhythmias,” says David H. Adams, MD, Marie-Joseé and Henry R. Kravis Professor and Chair of Cardiovascular Surgery, a principal investigator of the study. “Our research aims to provide novel mechanistic insights for further understanding the disease process and could impact future practice guidelines.”
In addition to Dr. Adams, the principal investigators in the study are Marc Miller, MD, Associate Professor of Medicine (Cardiac Electrophysiology); Zahi Fayad, PhD, Professor of Radiology, and Medicine (Cardiology), and Director of the BioMedical Engineering and Imaging Institute (BMEII), and Maria Giovanna Trivieri, MD, PhD, Associate Professor of Medicine (Cardiology), and Radiology.
In the United States, it is estimated that between 7 million and 9 million people have mitral valve prolapse, the most common form of valve disease. But Dr. Miller points out that only in recent years have physicians been widely aware of the risk of malignant arrhythmias in these patients. “Identifying patients at increased risk for developing life-threatening arrhythmias is especially important when you take into account the fact that many patients have no symptoms prior to suffering cardiac arrest,” says Dr. Miller.
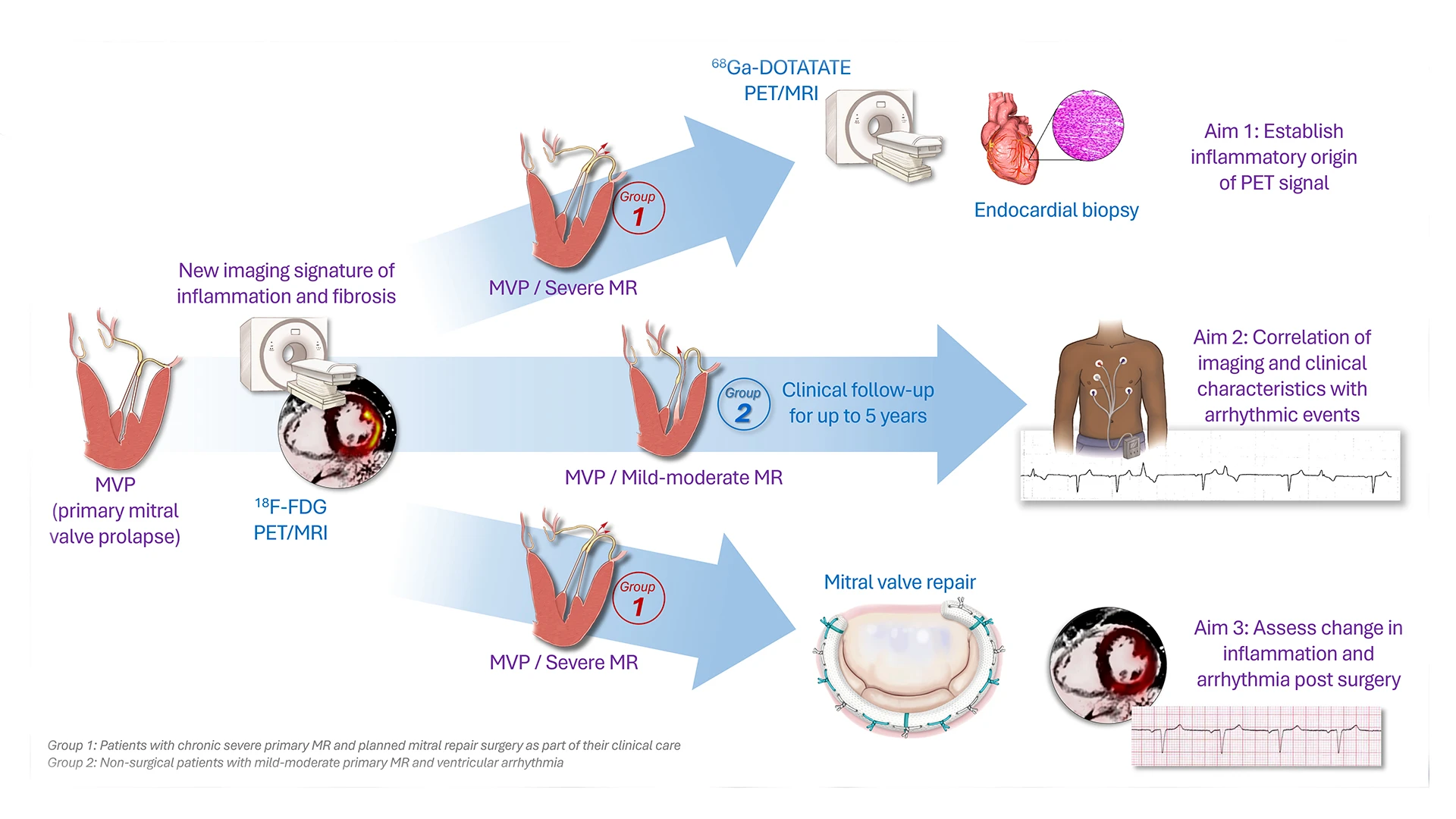
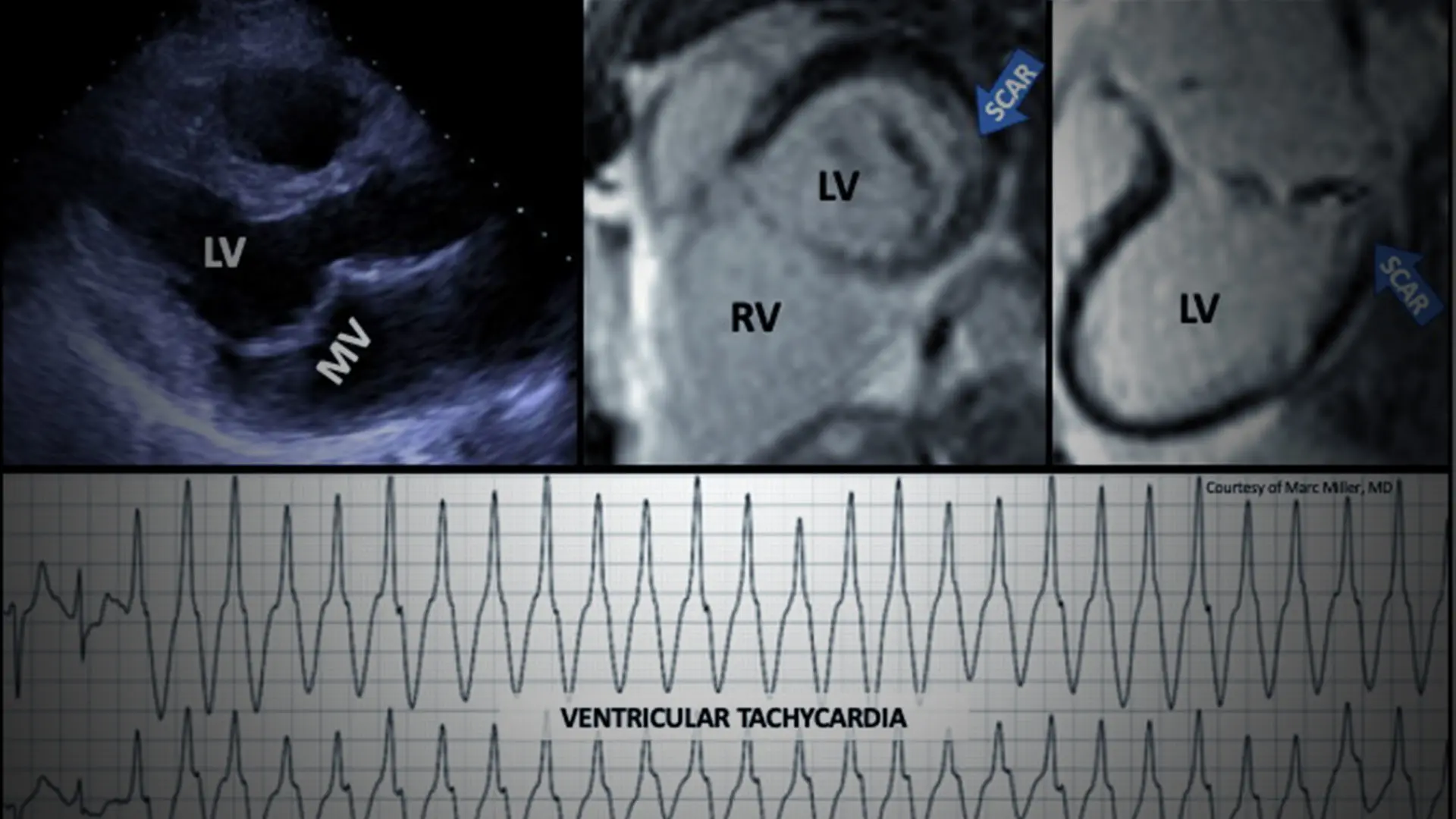
An abstract of the mitral valve prolapse research grant proposal.
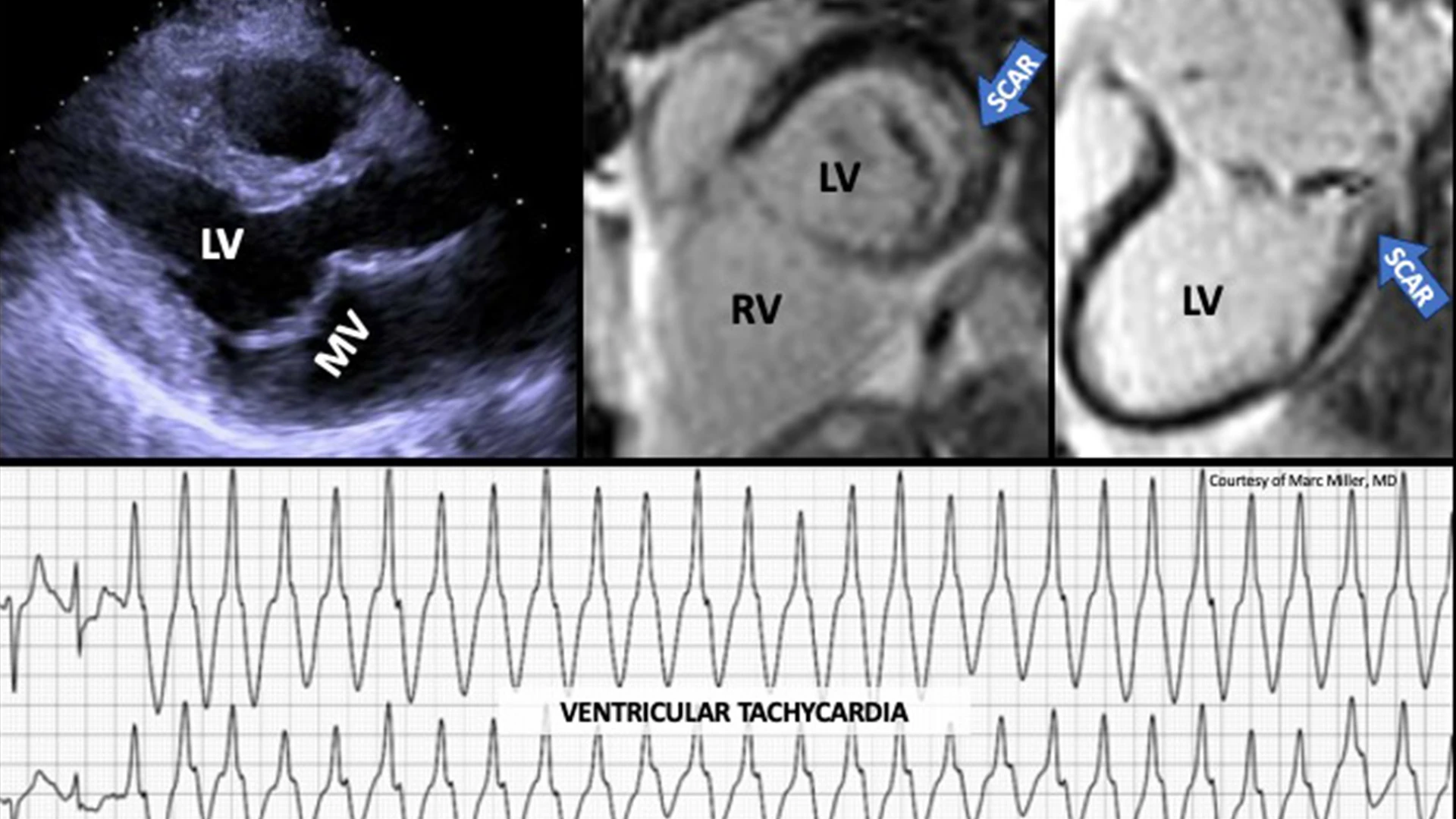
Images were obtained from a man in his mid-50s with asymptomatic degenerative mitral valve prolapse (bi-leaflet) with mild-moderate mitral regurgitation, who had an episode of syncope without prodrome. A subsequent ambulatory ECG monitor was notable for frequent salvos of ventricular tachycardia. Cardiac MRI imaging demonstrated replacement fibrosis (scar) in the basal infero-lateral left ventricle.
Even as the Mount Sinai team and others investigate this disorder, they called for increased awareness and vigilance by physicians and their patients. Specifically, it is now recommended that all patients with mitral valve prolapse have a routine electrocardiogram (ECG) during their annual mitral prolapse surveillance follow-up. If there is evidence of ventricular ectopy on the ECG or patient-perceived palpitations, it is advised to have an ambulatory ECG testing (Holter) periodically, to monitor the electrical activity of the heart continuously for one or more days. The goal is to capture and identify abnormal ventricular beats with a high risk for progression to more severe, sustained ventricular arrhythmias and potentially sudden cardiac death.
In December 2022, this precaution was recommended in a consensus statement of the European Heart Rhythm Association in collaboration with the European Society of Cardiology Council on Valvular Heart Disease and the European Association of Cardiovascular Imaging. This was endorsed by the Heart Rhythm Society, the Asia Pacific Heart Rhythm Society, and the Latin American Heart Rhythm Society.
The grant to Mount Sinai is a collaboration among four specialties: Cardiac Electrophysiology, Cardiology, Cardiovascular Surgery, and BMEII. The study is coordinated within the Mount Sinai Mitral Valve Repair Center, a quaternary reference center of excellence recognized by the American Heart Association and the Mitral Foundation for its demonstrated record of superior clinical outcomes of patients with mitral valve prolapse. One of the largest programs in the United States, the Center is led by Dr. Adams, Cardiac Surgeon-in-Chief of the Mount Sinai Health System.
The study also incorporates unique imaging technology provided by BMEII. “We are constantly developing novel imaging technologies and clinical applications to facilitate new ways to detect and characterize disease. The sensitive molecular information provided by PET imaging is a powerful complement to other imaging technologies, such as MRI and echocardiography, to understand complex pathology,” says Dr. Fayad.
Mount Sinai’s multidisciplinary research resources are crucial in the study of mitral valve prolapse and malignant arrhythmia, says Dr. Trivieri, Contact PI for the study. “The development of heart failure and arrhythmia may present differently in different patients with mitral valve prolapse,” she says. “Developing new indicators that are specific to predicting malignant arrhythmias and understanding what they mean over the long term will allow us to better care for our patients.”
Public attention was drawn to this condition in 2020, when Eleanor Carol Leavell Barr, the wife of Kentucky Congressman Andy Barr, died during a Zoom call, and an autopsy revealed the cause of the 39-year-old’s unexpected passing: undiagnosed mitral valve prolapse. The Cardiovascular Advances in Research and Opportunities Legacy (CAROL) Act, named for the congressman’s late wife, authorized critical investments in federal research that funded the grant to Mount Sinai.
“Long considered benign in many cases, mitral valve prolapse is now recognized as a more significant risk factor in sudden cardiac death,” Dr. Miller says. “We are now closer to understanding which patients are truly at higher risk.”
Featured

David H. Adams, MD
Marie-Josée and Henry R. Kravis Chair of Cardiovascular Surgery, Icahn School of Medicine, and Cardiac Surgeon-in-Chief, Mount Sinai Health System

Marc Miller, MD
Associate Professor of Medicine (Cardiology), Icahn School of Medicine at Mount Sinai
Maria Giovanna Trivieri, MD, PhD
Associate Professor of Medicine (Cardiology, and Radiology

Zahi Fayad, PhD
Lucy G. Moses Professor in Medical Imaging and Bioengineering, and Professor of Medicine (Cardiology)