Heart failure patients who are unvaccinated against SARS-CoV-2, the virus that causes COVID-19, were observed to have a threefold higher likelihood of death if infected with the virus, compared to fully boosted heart failure patients, according to a study led by Anuradha Lala, MD, Director of Heart Failure Research and Associate Professor of Medicine (Cardiology) at the Icahn School of Medicine at Mount Sinai.
The study, published in June 2022 in the Journal of Cardiac Failure, was the first to look at COVID-19 vaccination status and outcomes in patients with heart failure and indicated significant protective effects in this high-risk patient population.
“I launched this study because our heart failure patients often express fear of getting the COVID-19 vaccine after hearing reports of vaccine-related myocarditis, which could theoretically cause another cardiac setback for them,” says Dr. Lala, senior author of the study. “Until now, it has been difficult to explain to these patients how the cardiovascular benefits of vaccination substantially outweigh the risks of complications to them, because we didn’t have concrete evidence to show the substantial risks of being unvaccinated specific to this high-risk population.”
Mount Sinai researchers conducted a retrospective study to analyze the impact of COVID-19 vaccination status in the heart failure patient population. All Mount Sinai patients with diagnoses of heart failure (identified via electronic health record phenotyping) who made visits to Mount Sinai between January 1, 2021, and January 24, 2022, were included. Patients who had a heart transplant or left ventricular assist device were excluded.
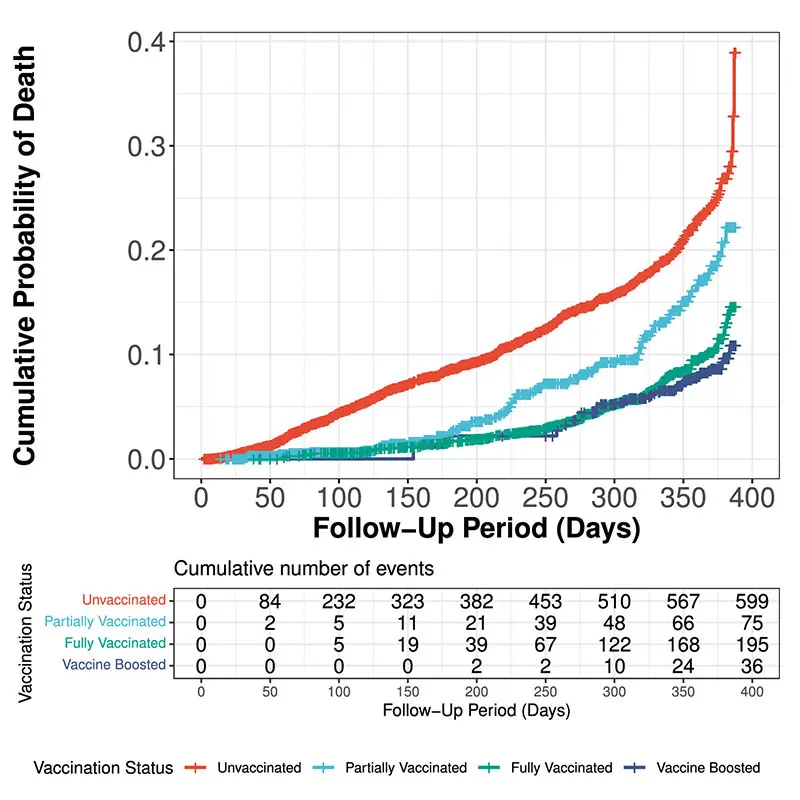
The cumulative incidence curve for mortality, stratifiedby vaccination status.
Of 7,094 patients with heart failure, 645 (9.1 percent) were partially vaccinated, 2,200 (31.0 percent) were fully vaccinated, 1,053 were vaccine-boosted (14.8 percent), and 3,196 remained unvaccinated (45.1 percent) by January 2022. The mean age was 73.3, and 48 percent were female. Overall, 904 (12.7 percent) of 7,094 total patients died over the mean follow-up time of 276.5 days. Of these, 73.4 percent were unvaccinated or only partially vaccinated.
Researchers said limitations to the study were related to the rapid evolution of the of COVID-19 pandemic and the variants during the study period. Data was restricted to one albeit large, hospital system, and, thus, COVID-19 infection, hospitalization, or death in other hospital systems were not captured. In addition, the causes of hospitalization were unknown. Data concerning specific treatment for HF or COVID-19 also were not available.
However, the study indicated that in a large cohort of patients with heart failure, vaccination against COVID-19 was associated with a lower likelihood of all-cause hospitalizations and mortality. Vaccine-boosted status was associated with the lowest rates of hospitalization and mortality, followed by fully and partially vaccinated status, with the worst outcome observed in unvaccinated patients.
“The findings further emphasize that heart failure patients need to take vaccines seriously, and stresses the importance of receiving the full COVID-19 vaccination dosage, especially since our previous work shows those with heart failure are 2.5 times more likely to die from the virus if infected,” Dr. Lala says. “I have used these results to help educate reluctant patients, and in many cases, this has been effective in encouraging them and getting them to follow through with full vaccination. The hope is that cardiologists will use these results as a tool to help their patients and improve their chances of survival.”
Featured

Anuradha Lala, MD
Associate Professor of Medicine (Cardiology), and Population Health Science and Policy