Mount Sinai Heart in 2022 successfully piloted a custom mobile application to streamline the transfer of heart attack patients from Mount Sinai Queens Emergency Department to The Mount Sinai Hospital. The application was developed by a multidisciplinary team of nurses, physicians, and other Mount Sinai team members to meet the time guidelines outlined in the American Heart Association’s Mission: Lifeline initative to advance care for patients during acute high-risk cardiac events.
The app, called STEMIcathAID, focuses on patients with an ST-segment elevation myocardial infarction (STEMI) who need percutaneous coronary intervention (PCI). Timing is critical in restoring blood flow to the blocked heart arteries of these patients and preserving heart muscle function. Outcomes are significantly better if the PCI is performed by experienced interventionalists at a tertiary facility, such as the Cardiac Catheterization Laboratory at The Mount Sinai Hospital.
Annapoorna Kini, MD, Director of the Cardiac Catheterization Laboratory, is leading the initiative to expedite such care in the Mount Sinai Health System. She designed the application and worked with an app developer to help launch STEMIcathAID.
“Since the application’s go-live in July 2021, the Cath Lab has seen a dramatic improvement across the board, says Dr. Kini, the Zena and Michael A. Wiener Professor of Medicine at the Icahn School of Medicine at Mount Sinai. “Patients have been consistently leaving the Mount Sinai Queens ED faster outbound to the Mount Sinai Hospital Cath Lab, and handoffs have been seamless with the new ability to anticipate the patient’s arrival through GPS tracking of the ambulance and communicate instantly as one large care team centered around the patient.”
The team presented the results of the pilot in 2022 at the Transcatheter Cardiovascular Therapeutics (TCT) conference and the European Society of Cardiology Congress. The primary metric for all patients was time from the patient’s first medical contact to PCI treatment. According to the American Heart Association, the goal is treatment within 120 minutes for patients requiring transfer from another hospital.
A Journal of the American Medical Association (JAMA) review of more than 25,000 transfer cases reported that only 17 percent of those cases met the AHA’s 120-minute metric. The JAMA paper said this metric has a significant impact on patient outcomes: in-hospital mortality for patients who met the 120-minute metric was significantly lower, with an adjusted odds ratio of 0.44 compared with patients who did not meet the metric.
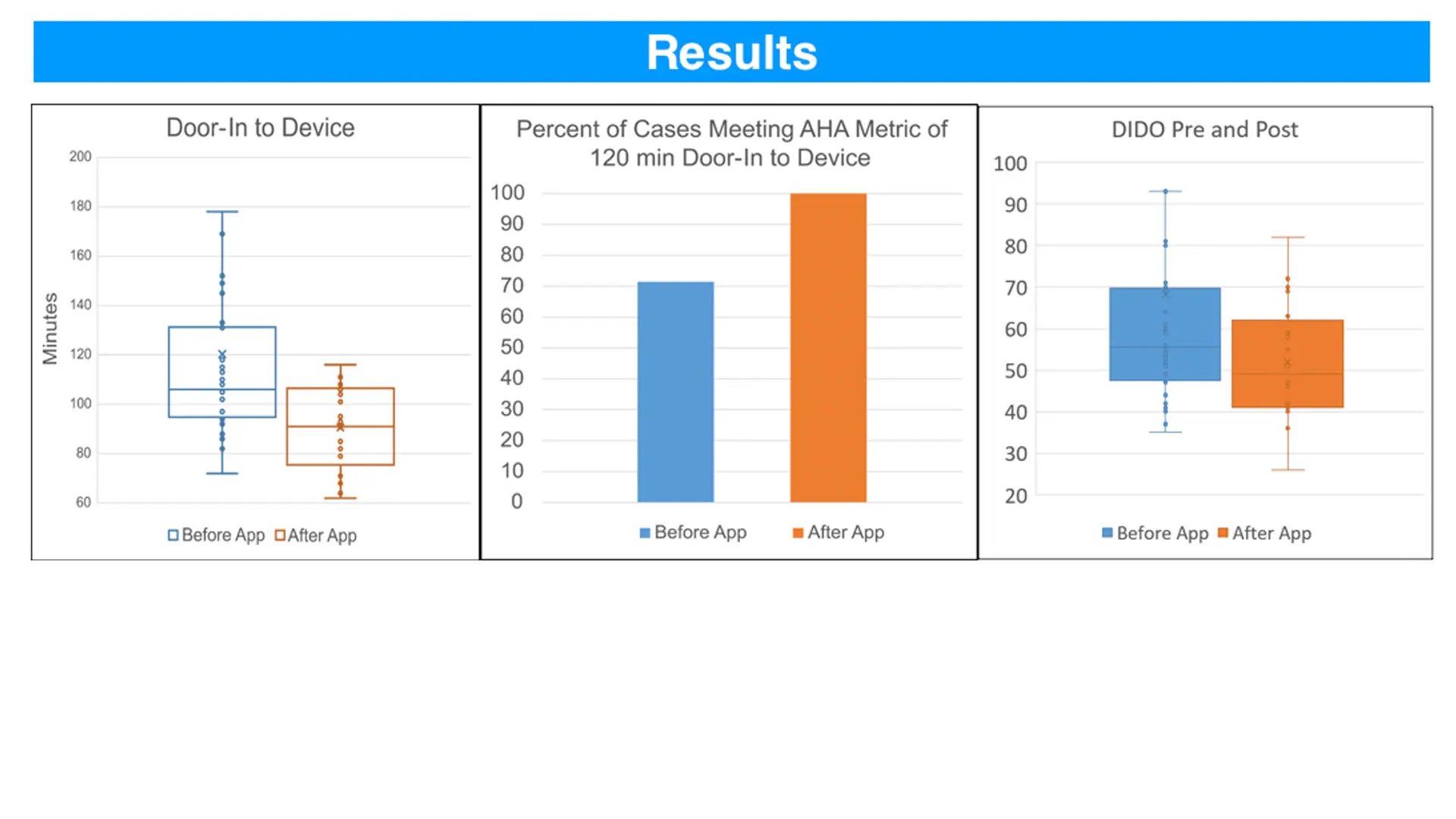
Even before the STEMI app went live, 71 percent of transfers from Mount Sinai Queens to The Mount Sinai Hospital met the 120-minute metric. But during the pilot, 100 percent of the transfers were completed in 120 minutes or less.
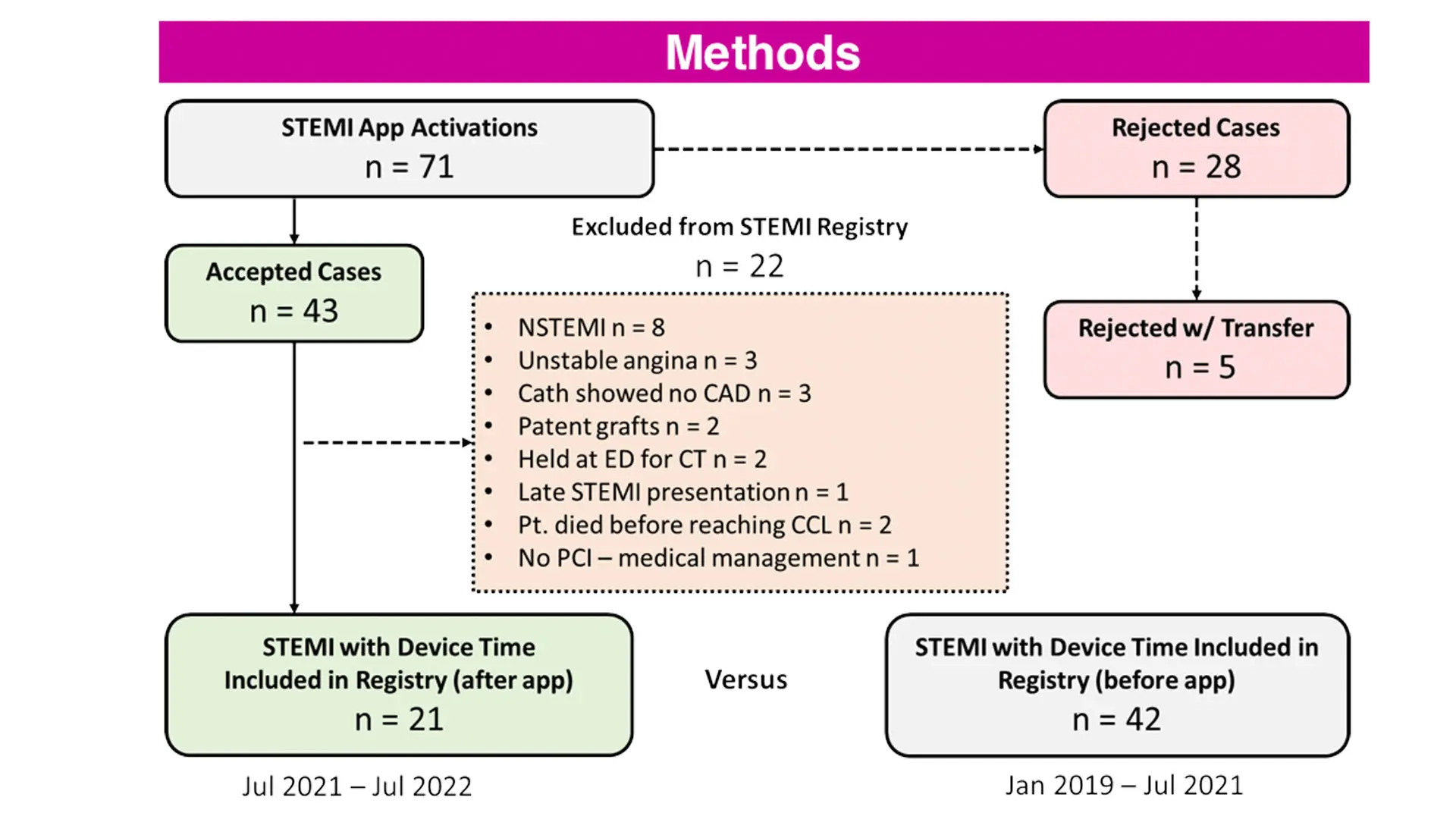
The app provides a digital platform for communication between STEMI care team members, immediate EKG transmission and interpretation, activation of the Cardiac Catheterization Laboratory, and ambulance tracking. During the pilot period from July 2021 to July 2022, a total of 71 suspected STEMI cases were activated through the app. Forty-three cases were accepted for transfer, and 28 cases rejected. After excluding patients who had normal coronary arteries, were intubated, expired in the Emergency Department, or had delays for transfer, the final study population included 21 STEMI cases. The team compared the door-to-device and door-in-door-out (DIDO) times for these patients with 42 STEMI cases who were activated through the traditional pathway from January 2019 to July 2021, before the app launch.
After implementing the app, the mean door-to-device time for STEMI transfer decreased from 120 ± 48 minutes to 91 ± 17 minutes . This significant improvement, of 29 minutes or 24 percent, resulted in all STEMI cases meeting the AHA goal of door-to-device time of 120 minutes or less. In addition, there was a decrease in mean DIDO time—the time from arrival to discharge at the STEMI referral hospital—from 68 ± 44 minutes to 52 ± 14 minutes after integrating the app into STEMI workflow.
“Using the STEMIcathAID application with the cooperation and dedication of our doctors, nurses, technicians, and transfer services, we have significantly improved our ability to care for the vulnerable heart attack patients in our community,” Dr. Kini says. “With a health care team dedicated to pushing the field forward, new technologies, and gold-star registry ratings, patients can rest easier in our care.”
The success of the pilot has demonstrated the benefit such a targeted, specialty tool can have in a complex and time-sensitive treatment pathway, the team reported. The STEMI app is being evaluated for a larger, deployment, where it would help with transfers in the larger Mount Sinai Health System and its network of cath labs and non-PCI-capable hospitals.
More information about the STEMIcathAID app is available here.
From left: Amit Hooda, MD; Isha Ranadive, MD; George Dangas, MD, PhD; Raman Sharma, MD; Andriy Vengrenyuk, MS; Annapoorna Kini, MD; Sahil Khera, MD; Visual Kapur, MD; Gregory Serrao, MD; Joseph Sweeny, MD; and Parasuram Krishnamoorthy, MD.
