An updated risk score can help predict possible contrast-associated acute kidney injury (CA-AKI)
among patients undergoing percutaneous coronary intervention (PCI), according to Mount Sinai
Heart researchers, led by Roxana Mehran, MD, Director of Interventional Cardiovascular
Research and Clinical Trials at the Icahn School of Medicine at Mount Sinai.
The team said the simple and unique assessment tool can enhance management of patients at
high risk of CA-AKI before, during, and after PCI, and improve their prognosis following the
procedure.
The metric, called the Mehran-2 CA-AKI Risk Score, was developed by Dr. Mehran,
Professor of Medicine (Cardiology), and Population Health Science and Policy, along with other
Mount Sinai cardiologists. Their results were presented in November 2021 at the American Heart
Association Scientific Sessions, with simultaneous publication in The Lancet.
In PCI, interventionalists use angiography to determine which coronary arteries have the most
severe blockages, and inject iodinated contrast into the bloodstream to make the blockages
visible on X-ray. That fluid is toxic, and high-risk groups can have kidney problems as a result.
The new risk score expands upon the initial risk score developed by Dr. Mehran in 2004 that has
been implemented in cardiac catheterization labs around the world. The updates take into
account changes in practice surrounding PCI, including more advanced imaging techniques that
require less toxic contrast agents, as well as improved stents.
“Although the incidence of CA-AKI has decreased over the past few years, it remains a
significant complication of PCI and is associated with mortality, prolonged hospital stay, and
increased medical costs. As the number of high-risk patients undergoing PCI increases every
year, it is really crucial to risk-stratify these patients to optimize outcomes and minimize
cardiorenal complications,” explains Dr. Mehran. “Simple measures can be taken around the
time of procedure when a patient is identified to be at high risk of CA-AKI, and we hope this
new score is widely adopted to enhance the care of patients and improve outcomes.”
“Although the incidence of CA-AKI has decreased over the past few years, it remains a significant complication of PCI and is associated with mortality, prolonged hospital stay, and increased medical costs.”
- Roxana Mehran, MD
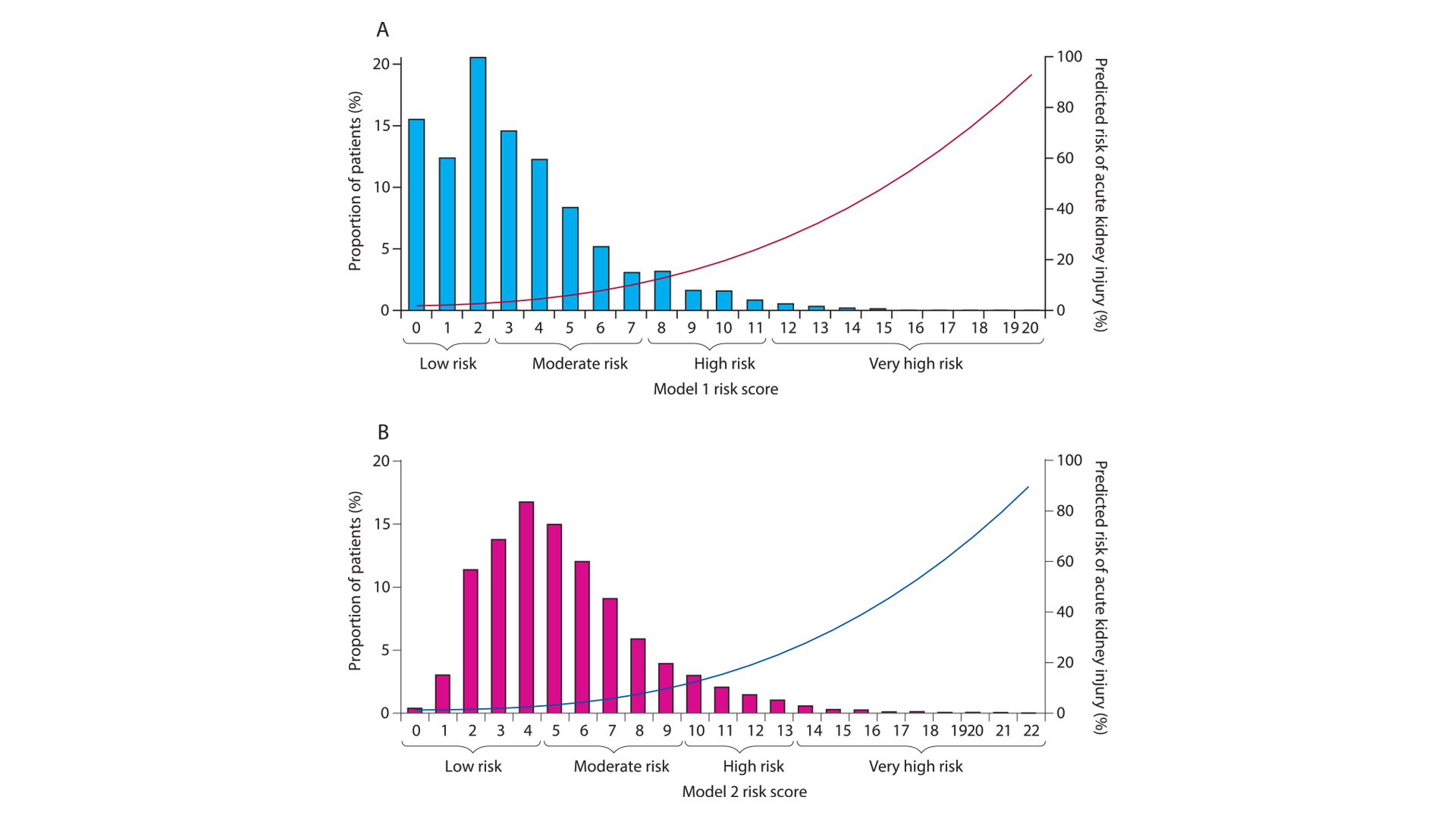
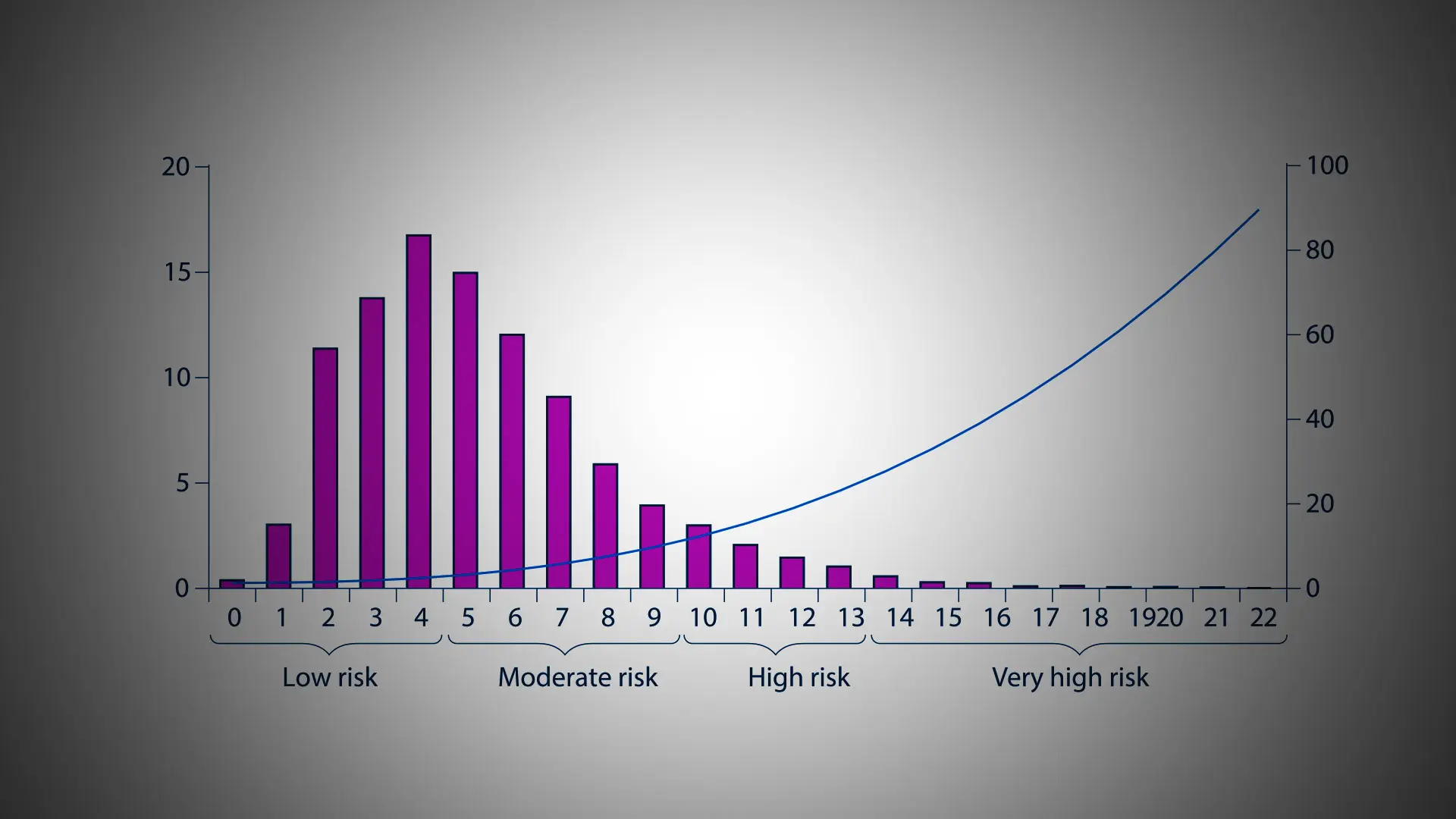
Risk of contrast-associated acute kidney injury in the derivation cohort according to risk score values from (A) Model 1 and (B) Model 2. Bars show proportion of patients, and lines show the predicted risk of acute kidney injury.
Dr. Mehran and her team created a predictor model identifying which patients are at highest risk
of acute kidney injury based on baseline risk factors, which included diabetes, anemia,
congestive heart failure, advanced kidney disease, acute heart attack, and ST-segment elevation
myocardial infarction (STEMI), or complete blockage of a major heart artery. Being older than
75 was also considered a risk factor. They assigned an individual score to each of those risk
factors, then calculated patients’ overall risk scores, putting them in specific groups: between 0-4
was “low risk,” 5-9 was “moderate risk,” 10-13 was “high risk,” and anything above 14 was
“extremely high risk.”
By calculating patients’ risk scores, doctors can modify their periprocedural management
approach to improve outcomes. This may include increasing hydration before PCI, administering
statins, and minimizing the amount of contrast used during the procedure. The risk score may
also help doctors increase monitoring before and after PCI, potentially doing additional blood
tests. More specifically, if a patient is low risk, doctors can measure creatinine level once after
the procedure, compared to high-risk patients, who may need several measurements.
“Acute kidney injury after invasive procedures remains a mystery since it has such a robust
adverse prognosis, yet we still don’t know of a clear responsible mechanism. Therefore, it
remains a very challenging and interesting research field,” explains senior author George
Dangas, MD, PhD, Professor of Medicine (Cardiology) and Director of Cardiovascular
Innovation at the Zena and Michael A. Wiener Cardiovascular Institute at Icahn Mount Sinai.
“The fact that periprocedural events have only minor contribution to the overall predictive power
makes this model even more important, as its risk assessment is accurately available before the
start, and plans can be made very early on.”
“We plan to design clinical trials and incorporate this score to evaluate both external validation in predicting acute kidney injury but also clinical outcomes,” adds Dr. Mehran.
Featured
Roxana Mehran, MD
Professor of Medicine (Cardiology) and Population Health Science and Policy, and Director of Interventional Cardiovascular Research and Clinical Trials at the Zena and Michael A. Wiener Cardiovascular Institute