The Ross procedure may be a more favorable option for aortic valve replacement among patients under 50 years old than more standard mechanical or biological replacements, according to a study from Mount Sinai Heart. The research, published in the February 2022 issue of the Journal of American College of Cardiology, is the first to compare the Ross procedure to the other options, and shows that it leads to improved survival and better outcomes in younger adults.
“Not only was survival better than after biological or mechanical aortic valve replacement, it was also identical to the matched U.S. general population. To this day, this is the only operation that has ever been shown to restore survival after aortic valve replacement in young adults,” says lead author Ismail El-Hamamsy, MD, PhD, the Mount Sinai Randall B. Griepp, MD Professor of Cardiovascular Surgery at the Icahn School of Medicine at Mount Sinai and Director of Aortic Surgery for the Mount Sinai Health System. “This demonstrates the impact of valve choice in the long term. However, there is an important word of caution: the Ross procedure is a more complex operation and should only be performed in Ross centers of excellence. When done in that setting, this represents a major breakthrough for young patients with aortic valve disease, including young women contemplating pregnancy.”
The standard open-heart procedures for repair include mechanical valve replacement—which requires patients to take lifelong blood thinners to prevent stroke, as well as make some lifestyle modifications such as avoiding contact sports or activities that may lead to falls and bleeding—or a biological aortic valve replacement from a human or animal donor, which are hampered by limited durability in younger patients. The Ross procedure is a more complex operation where a surgeon replaces the diseased aortic valve with the patient’s own living pulmonary valve.
“Not only was survival better than after biological or mechanical aortic valve replacement, it was also identical to the matched U.S. general population.”
- Ismail El-Hamamsy, MD, PhD
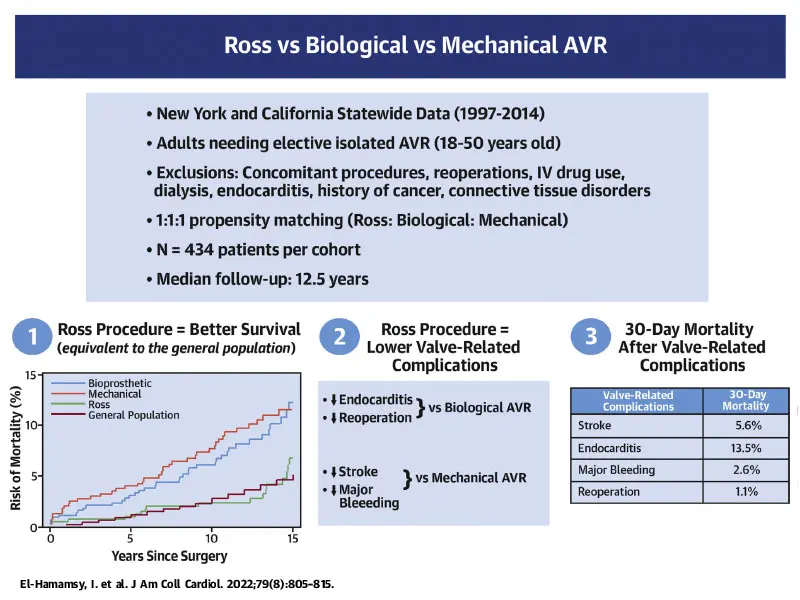
Researchers analyzed records of 1,302 patients between 18 and 50 years old who underwent first-time elective aortic valve replacement surgery in California and New York State between January 1, 1997, and December 31, 2014. Patients were equally divided into three categories using propensity-matched analysis to eliminate any baseline differences; one-third of them had the Ross procedure, one-third had biological valve replacement, and the rest had mechanical valve replacement. The retrospective study compared the long-term survival and risk of valve-related complications (including stroke, major bleeding, reoperation, and acute endocarditis) according to the surgical procedure.
Investigators looked at outcomes 15 years post-procedure and found that patient survival was significantly better after the Ross procedure. At 15 years, overall mortality was more than twofold higher if the patients received a biological or mechanical aortic valve versus a Ross procedure. Furthermore, survival after the Ross procedure (93 percent survival at 15 years) was identical when compared to people of the same age and sex in the U.S. general population who did not have aortic valve replacement surgery.
In terms of valve-related complications, the Ross procedure was associated with a significantly lower risk of stroke or major bleeding than a mechanical valve (3.8 percent after a Ross procedure versus 13 percent after a mechanical valve at 15 years). Similarly, the Ross procedure was associated with significantly fewer reoperations (17 percent versus 30 percent at 15 years) and endocarditis than a biological valve (2.3 percent versus 8.5 percent at 15 years). At 15 years, however, the risk of reoperation was higher after a Ross procedure than after mechanical valve replacement (17 percent versus 7.4 percent at 15 years).
The study also looked at 30-day mortality after the occurrence of any valve-related complication, including stroke, major bleeding, endocarditis, or reoperation. Researchers found the lowest mortality was linked to reoperation (1 percent), whereas if patients had a stroke, major bleeding, or endocarditis, the associated mortality was at least three times higher (5.6 percent after a stroke and 13.5 percent after endocarditis).
“This study demonstrates that while there is a definite risk of reoperation after the Ross procedure, the associated risk is low. In other words, this should be seen as a bump on the road, rather than the end of the road. In contrast, if patients suffer a stroke, hemorrhage, or infection, the consequences are much more dire,” explains Dr. El-Hamamsy. “Patients should be given all this data so they can make truly informed decisions about these major life events. Ultimately, the Ross procedure is associated with better survival and fewer complications.”
The authors hope that this will further encourage the development of regional Ross centers of excellence to improve patient access and safety. In addition to surgical expertise, this involves cardiologists with valve expertise, dedicated cardiac anesthesia and ICU, as well as multimodality imaging, all of which are present at Mount Sinai. Presently, Dr. El-Hamamsy and his team, which has the largest experience worldwide with this operation, are working on further improving the durability of the Ross procedure so that even fewer patients ever need reoperations.
Featured
Ismail El-Hamamsy, MD, PhD
Randall B. Griepp Professor of Cardiovascular Surgery, Icahn School of Medicine, and Director of Aortic Surgery, Mount Sinai Health System
Paul Stelzer, MD
Professor of Cardiovascular Surgery, Icahn School of Medicine
