Use of a novel technique called the quantitative flow ratio (QFR) to precisely identify and measure the severity of artery blockages can lead to significantly improved outcomes after percutaneous coronary intervention (PCI), according to a study done in collaboration with Mount Sinai faculty.
This research, which is the first to analyze QFR and its associated clinical outcomes, may lead to widespread adoption of QFR as an alternative to angiography or pressure wires to measure the severity of blockages, or lesions, in patients with coronary artery disease. The study results were announced in November 2021 as a late-breaking clinical trial at the Transcatheter Cardiovascular Therapeutics Conference, and simultaneously published in The Lancet.
“For the first time we have clinical validation that lesion selection with this method improves outcomes for patients with coronary artery disease undergoing stent treatment,” says senior author Gregg W. Stone, MD, Director of Academic Affairs for Mount Sinai Health System and Professor of Medicine (Cardiology), and Population Health Science and Policy, at the Icahn School of Medicine at Mount Sinai. “By avoiding the time, complications, and extra resources required to measure lesion severity using a pressure wire, this simpler technique should serve to greatly expand the use of physiology in patients undergoing cardiac catheterization procedures.”
Patients with coronary artery disease often undergo PCI, in which interventional cardiologists use a catheter to place stents in the blocked coronary arteries to restore blood flow.
Most doctors depend on angiography to determine which arteries have the most severe blockages, and use that visual assessment to decide which arteries to treat. This method is not perfect: some blockages may look more or less severe than they actually are, and doctors can’t precisely tell from the angiogram alone which blockages are most seriously affecting blood flow. Outcomes can be improved if lesions to stent are selected using a pressure wire to identify which are obstructing blood flow. But this measurement procedure takes time, can cause complications, and entails extra costs.
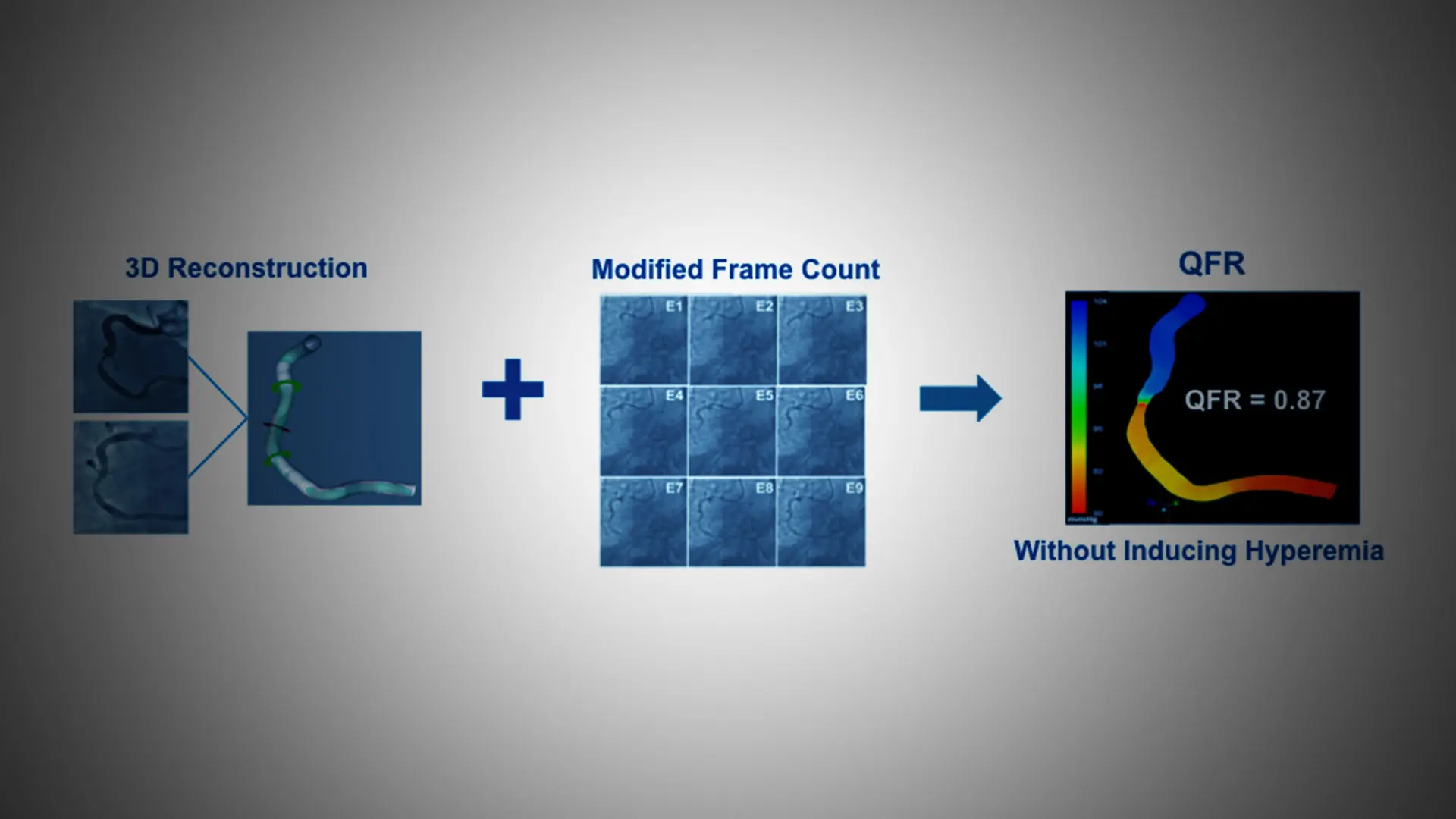
QFR technology uses 3D artery reconstruction and measurement of blood flow velocity that gives precise measurements of the pressure drop across a blockage, allowing doctors to make better decisions as to what arteries to stent during PCI.
“For the first time we have clinical validation that lesion selection with this method improves outcomes for patients with coronary artery disease undergoing stent treatment.”
- Gregg Stone, MD
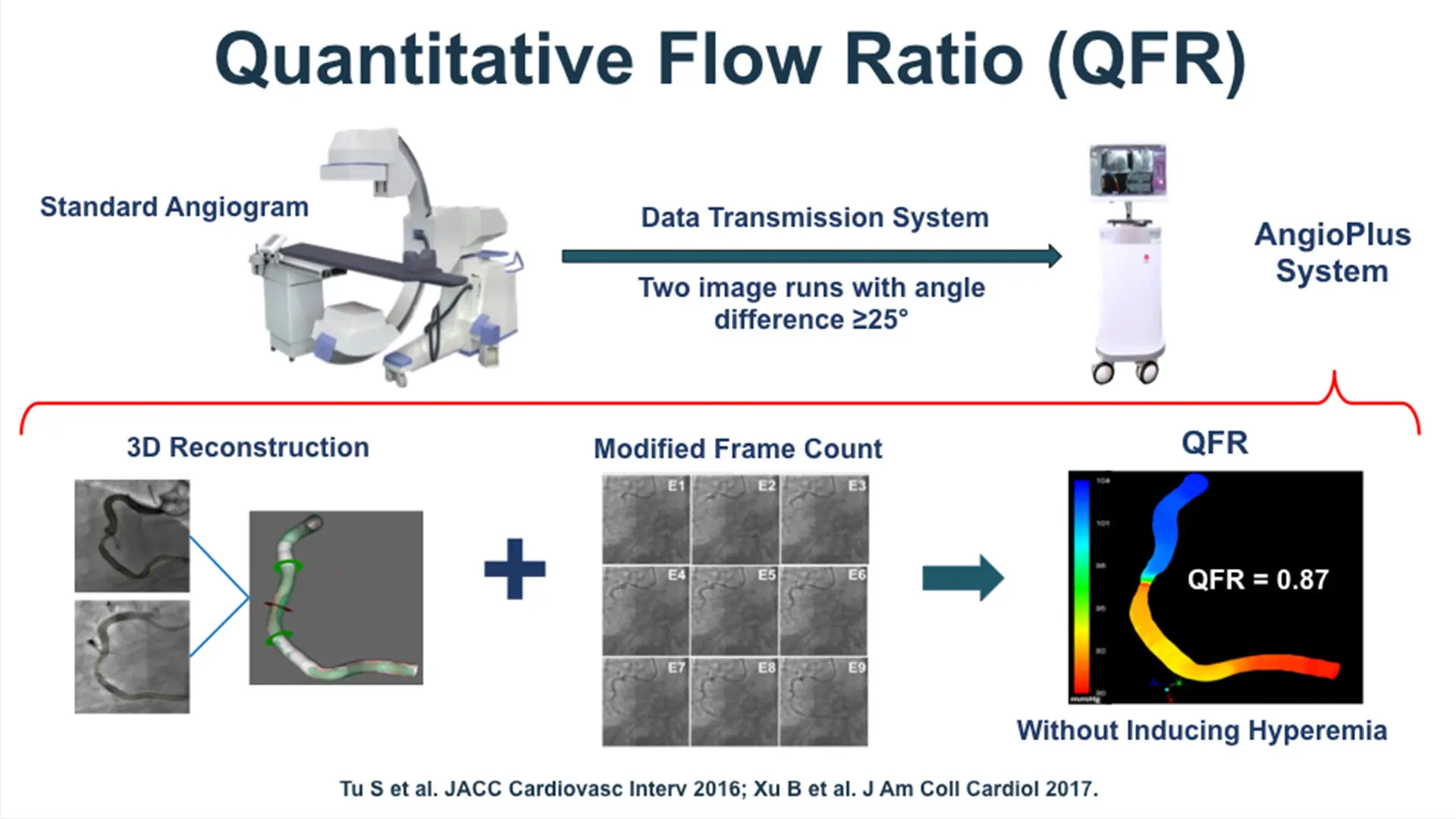
Quantitative flow ratio technology uses 3D artery reconstruction and measurement of blood flow velocity that gives precise measurements of the pressure drop across a blockage.
To study how QFR impacts patient outcomes, researchers conducted a multicenter, randomized, blinded trial of 3,825 participants in China undergoing PCI between December 25, 2018, and January 19, 2020. Patients either had a heart attack 72 hours prior, or had at least one coronary artery with one or more blockages that the angiogram measured as between 50 and 90 percent narrowed. Half of the patients underwent the standard angiography-guided procedure based on visual assessment, while the other half underwent the QFR-guided strategy.
In the QFR-guided group, doctors chose not to treat 375 vessels that were originally intended for PCI, compared to 100 in the angiography-guided group. The technology thus helped eliminate a greater number of unnecessary stents. In the QFR group, doctors also treated 85 vessels not originally intended for PCI compared to 28 in the angiography-guided group. The technology thus identified more obstructive lesions that would not have otherwise been treated.
As a result, patients in the QFR group had lower one-year rates of heart attack compared to the angiography-only group (65 patients vs. 109 patients) and a lesser chance of needing additional PCI (38 patients vs. 59 patients) with similar survival. At the one-year mark, 5.8 percent of patients treated with the QFR-guided PCI procedure had either died, had a heart attack, or needed repeat revascularization (stenting), compared to 8.8 percent of patients undergoing the standard angiography-guided PCI procedure, a 35 percent reduction. The researchers attributed these significant improvements in outcomes to QFR allowing doctors to choose the correct vessels for PCI and also avoid unnecessary procedures.
“The results from this large-scale blinded randomized trial are clinically meaningful, and similar to what would have been expected with pressure wire-based PCI guidance.” Dr. Stone says. “Based on these findings, following regulatory approval, I would anticipate QFR to be widely adopted by interventional cardiologists to improve outcomes for their patients.”
Featured
Gregg W. Stone, MD
Professor of Medicine (Cardiology), and Population Health Science and Policy