Nursing at Mount Sinai—always pivotal to clinical care and the patient experience—underwent transformative changes in 2020. Beth Oliver, DNP, RN, was appointed Senior Vice President and Chief Nursing Executive for the Mount Sinai Health System. With Dr. Oliver in this newly created role, nursing evolved throughout the COVID-19 crisis and created innovative processes that have improved the patient experience.
“Nurses are pivotal to the patient experience for several reasons,” Dr. Oliver says. “Nurses play the largest role in the day-to-day experience of our patients because of their frequent and personal interactions. Nurses are on the front lines every day, working tirelessly to care for patients and their families. Nurses are their patients’ best advocates—individualizing care to ensure the best possible clinical outcomes. By demonstrating effective communication, empathy and agility, nurses play a vital role in creating a positive patient experience and improving patient satisfaction scores.”
A national leader in cardiovascular care, Dr. Oliver has fostered and supported evidence-based, patient-centered care throughout her career. As Chief Nursing Executive, her top priorities are ensuring the safety and quality of care for patients; supporting and advancing the professional development of nurses; focusing the care provided on the needs of patients and communities; and ultimately, continuing to develop and maintain Mount Sinai’s national reputation for excellence in nursing services.
In 2020, she fostered a strong partnership between Nursing and the Office of Patient Experience (OPX) to help develop nurses as leaders and create environments that support their growth through initiatives including the Care Checks Committee, Patient Experience Coaching, and Narrating Care.
“Nurses are on the front lines every day, working tirelessly to care for patients and their families.”
Beth Oliver, DNP, RN
“The partnership between Nursing leadership and the Office of Patient Experience has been effective in increasing the engagement of nursing leadership as well as our front line nurses in patient experience improvement initiatives,” Dr. Oliver says. “Together, we have developed ways to increase awareness and transparency of patient experience data, improve the way we cascade information down to the front line, and create forums to share best practices from the unit level across the Health System.”
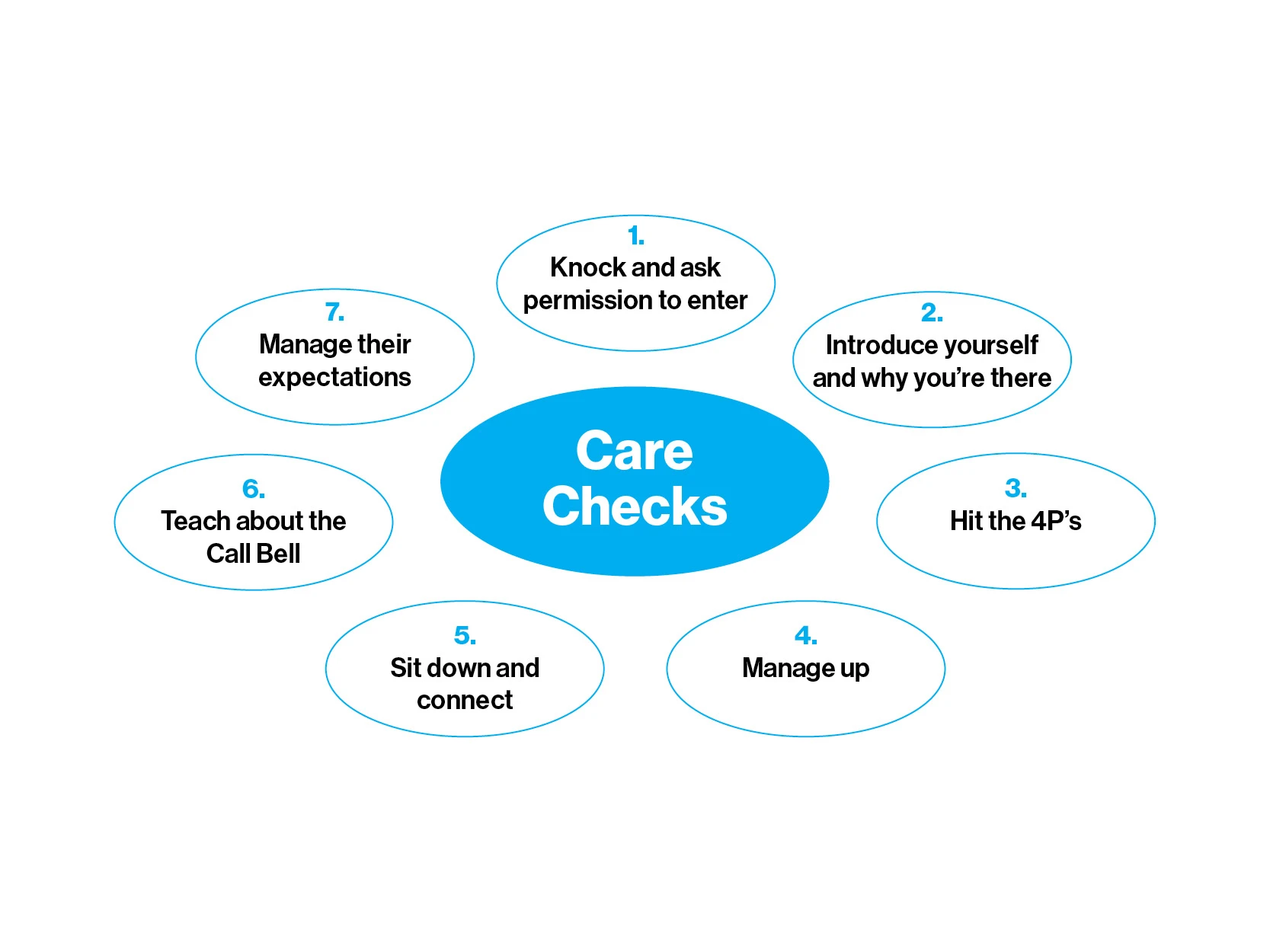
Dr. Oliver collaborated with OPX in establishing the Care Checks Steering Committee, which she co-chairs with Erica Rubinstein, MS, LCSW, CPXP, Vice President, Service Excellence and Patient Experience, Mount Sinai Health System. The committee invites nursing and patient experience leaders to share their best practices and their solutions to any barriers faced at the bedside.
As one principle of Mount Sinai Nursing says, “the bedside is the best side;” it is where patient safety and connection are prioritized. The Care Checks Committee supports a culture of nursing excellence, advancing strong nurse leaders by supporting the idea of shared governance. This work helps nurse managers understand the patient experience data, and allows them to become part of the solution. Building a strong connection among nurses throughout the system, the Committee became an important support system in 2020 as it shared clinical care and wellness strategies during the challenges of a global pandemic.
In another key initiative, Nursing and OPX deployed Patient Experience Coaches to support nursing across the Health System. These coaches partner with nurse managers to develop and enhance leadership skills in emotional intelligence, communication, giving and receiving feedback, conflict resolution, data literacy, and building effective teamwork on their units.
“Nursing is demanding and complicated work. When they stop and connect with a gentle and reassuring touch, a warm smile, a reassuring word, a moment to listen and empathize, they often make the unbearable, bearable. Nurses may never really know the extent of the impact of their kindness—it is their legacy,” says Sabrina Segui, MA, CPXP, a Patient Experience Coach. Nurse managers throughout the system have reported the impact of this coaching work, which has had proven success in supporting best practices in everyday patient care.
A “Narration of Care” Tip Sheet included Care Checks best practices for the bedside.
“I now focus less on scripting myself and instead allow a genuine connection with patients and families, which makes for a better and more impactful round,” says a nurse manager who works closely with her coach.
Units in which nurse managers received coaching had substantially higher positive rates of change in Nurse Communication and Teamwork (as measured by HCAHPS) than units that did not receive coaching. The rate of change achieved in coached units is on par with the rates of improvement achieved by the top 30 percent of organizations across the nation.
“I am more comfortable and confident in coaching, providing feedback, and having crucial conversations with my staff,” says a nurse manager. “Coaching has also strengthened my patient rounding. My coach taught me the importance of asking questions to understand what is most important to the patient and provided me with the tools to do so.”
Patient Experience Coaches have also made great strides in focusing efforts in Narrating Care, a best practice that is proven to increase patient experience scores and benefit the patient’s overall experience. Narrating Care is defined as explaining to patients what is being done, how and why, and what the patient can expect.
“By narrating care, we keep our patients and families informed,” Ms. Segui says, “which reduces their anxiety and confusion, improves patient literacy, builds trust and confidence in the nurses’ competence, and nurtures a more collaborative relationship. This improves patients’ compliance with medications and care, and opens up communication.”
Narration of care is also useful when practiced by nonclinical team members, such as housekeeping staff, dietary, environmental services, and security. “Very often patients tell us the EVS personnel were the ones that were the friendliest and made them feel comfortable. Their connection and empathy with the patients make a meaningful and lasting impression on our patients and their loved ones,” Ms. Segui says.
Narrating care involves using open-ended questions for accurate understanding and encouraging the patients to think broadly and deeply, so nurses can meet their needs and provide the best possible care. Research shows that although nurses report consistently narrating care to their patients, the patients report otherwise. This difference in perception led to a deeper investigation by Nursing and OPX and a renewed focus on effectively narrating care to patients so that it is not only done, but it is felt by the patient being cared for.
“Our nurses are absolutely pivotal to the patient experience. We can’t thank them enough for their passion to do right by our patients every day,” Ms. Rubinstein says. “We always look forward to partnering with Dr. Oliver to elevate nursing, continuing to support their needs, advance them as leaders, and ultimately remove any barriers in their way to connecting with and healing our patients. They are the patient experience.”
A video demonstrates and discusses the best practices for Narrating Care.
Our patients, in their own words
“Top notch nurses. I was there immediately prior to the COVID-19 crisis, and it was clear
that everyone was anxious and bracing for the onslaught, but they were thoughtful and
caring—many times working through lunch and going the extra mile to get my meds.”
- Mount Sinai Hospital inpatient
Featured

Judy H. Cho, MD,
Dean of Translational Genetics, and Director, The Charles Bronfman Institute for Personalized Medicine

Shikha Nayar, PhD,
Postdoctoral Fellow